AHA 2021丨AMAZE研究:与单独肺静脉隔离相比,使用 LARIAT 辅助左心耳结扎术的结局
2021-11-18 苏彦宾 郭一凡 “心关注”公众号
在房颤患者的射频消融治疗中,左心耳(LAA)因其独特的解剖与电生理特性始终扮演着重要的角色,在LAA内形成的血栓是绝大多数(约90%)卒中的原因。
2021年11月14日,2021年美国心脏协会(AHA)科学年会公布了AMAZE试验的研究结果,该研究旨在评估房颤患者射频消融治疗中使用LARIA装置进行左心耳(Left atrial appendage,LAA)结扎作为肺静脉窦隔离术(Pulmonary Vein Antral Isolation , PVAI)辅助治疗的附加疗效:能否安全降低初始消融治疗后12个月房颤复发率。结果表明:LARIAT装置安全有效的结扎了LAA,对于接受房颤消融治疗的持续性房颤总体人群,在减少房颤复发性心律失常方面,辅助LAA结扎并不优于单独肺静脉窦隔离;探索性分析表明,在早期持续性房颤和左心房体积较大的亚组中,LAA结扎辅助治疗有可能提供更好的节律控制。
研究背景
AHA 2021丨AMAZE
在房颤患者的射频消融治疗中,左心耳(LAA)因其独特的解剖与电生理特性始终扮演着重要的角色,在LAA内形成的血栓是绝大多数(约90%)卒中的原因。为了降低卒中风险,有效隔绝左心耳防止其形成血栓已经成为房颤患者治疗中的重要一环,由于外科手术隔绝左心耳的成功率并不理想,目前常用的左心耳隔绝装置包括两种经皮LAA消除技术:心内膜LAA闭合/堵塞(Watchman, Amplatzer装置)以及本研究中体导的心外膜LAA结扎(LARIAT)装置。大量的研究探索了LARIAT装置对左心耳结扎的疗效,已经对其安全性和有效性有了相当的肯定。LAA在房颤患者,特别是那些持续性和长程持续性房颤患者中的致心律失常作用已被认识,BELIEF研究证实了增强对LAA的消融和电隔离可以有效减少随访中房颤复发率,但由于电隔离后LAA运动下降,血栓形成的风险增加,患者需要长期维持抗凝治疗。而LARIAT闭合LAA时,LAA电压[1]出现明显降低或完全消除。综上所述LARIAT结扎似乎是一种潜在的既可以实现电隔离,又可以预防卒中的治疗方案。目前已有小型研究[2,3]表明,LAA与LARIAT结扎可终止持续性心房颤动,并可能提高消融成功率,但尚无大型RCT研究对其结果进行进一步证实。基于此背景,本研究将在一项大型随机多中心临床试验中探索LARIA装置进行左心耳(Left atrial appendage,LAA)结扎作为肺静脉窦隔离术(Pulmonary Vein Antral Isolation, PVAI)辅助治疗能否安全降低初始消融治疗后12个月房颤复发率。
研究设计
AHA 2021丨AMAZE
AMAZE研究是一项前瞻性、多中心、随机对照研究,共纳入了2015年9月至2021年4月期间,美国51个中心的610例患者,并以2:1的比例随机分组,一组进行LARIAT装置对左心耳结扎后行PAVI治疗,一组只进行PAVI,具体分组及随访情况如图1所示。两组患者均按严格的设计方案执行PVAI,PVAI以外的LA病变考虑方案偏差;病灶设置现场监测和跟踪。观察终点包括主要疗效终点、主要安全终点及技术成功率,其中主要疗效终点包括PVAI后12月无复发房性心律不齐(atrial arrythmias,AA),无新的I类或III类AAD药物使用或增加剂量,AA定义为持续> 30秒的心房颤动、心房扑动或房性心动过速,心率评估使用24小时动态心电图和症状事件监测。主要安全终点包括与性能目标(PG)相比,预先确定的LARIAT后30天严重不良事件的组合。技术的成功是指成功放置LARIAT,实现有效的LAA结扎(≤1±1mm直径残余心房通道)。
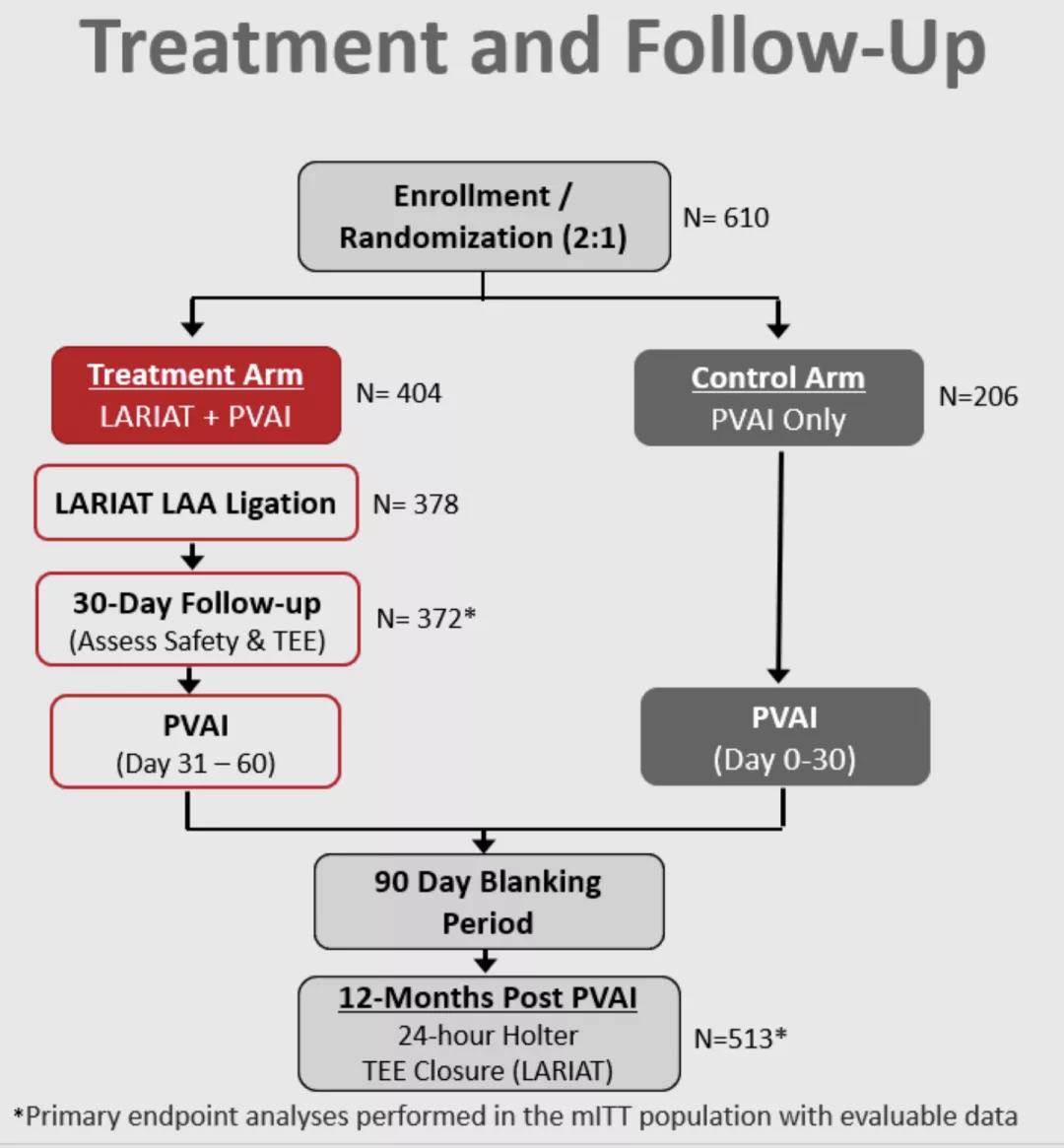
图1:研究设计流程图
研究结果
AHA 2021丨AMAZE
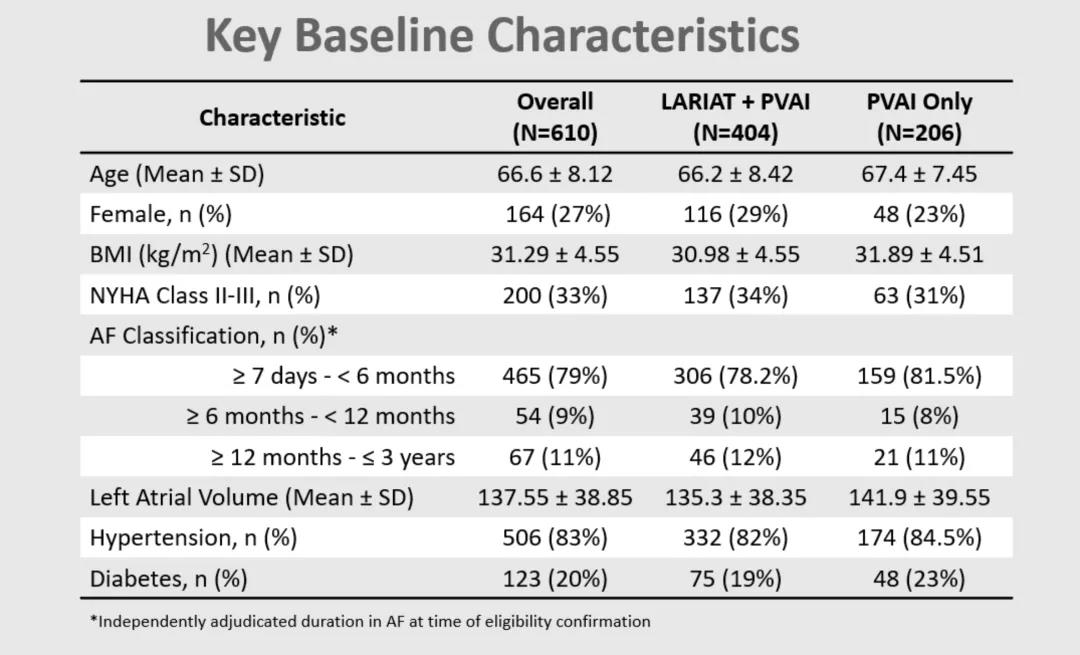
1、基线特征
两组在基线特征方面保持良好平衡(表1)。大多数患者是老年男性,BMI均偏高,两组人群房颤分型比例无显着差异,高血压普遍存在,糖尿病患病率较低。
表1: 两组患者主要基线特征
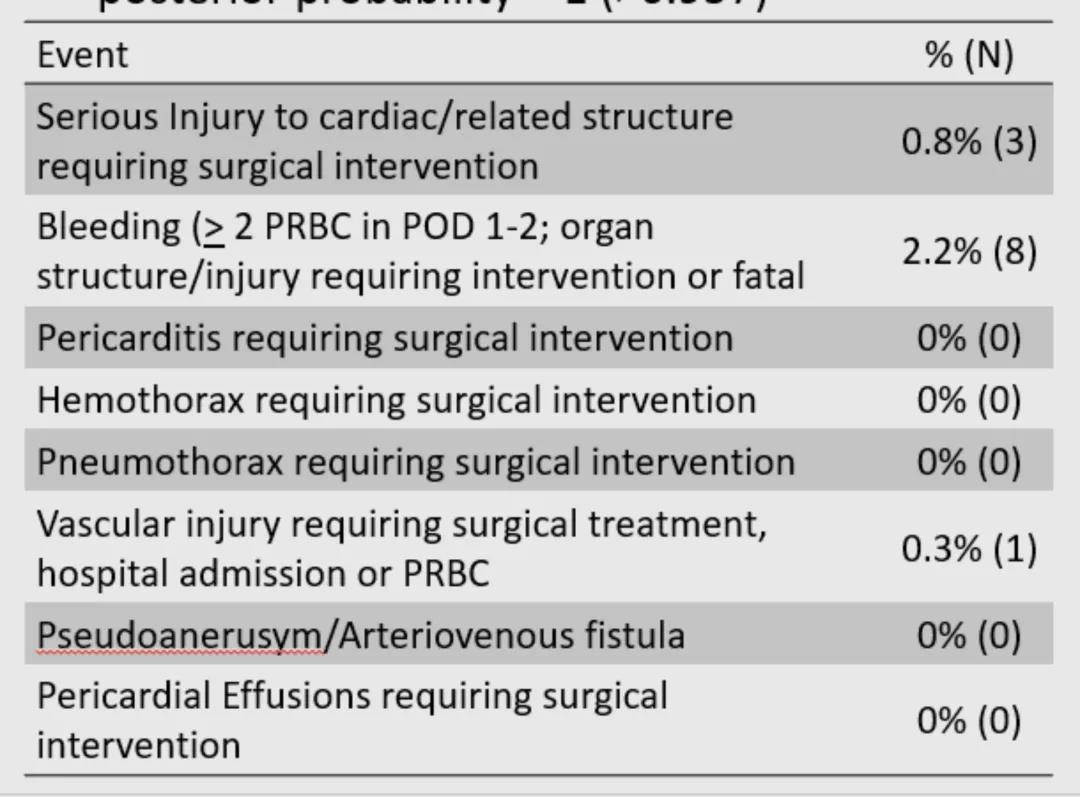
2、主要安全终点事件及技术成功(LAA结扎)
LARIAT后30天的主要安全终点率为3.4%(<10% PG);[95% Bayesian CI:2.0, 5.0]主要安全终点满足Bayesian后验概率= 1(>0.957)(表2)。
表2: 安全终点
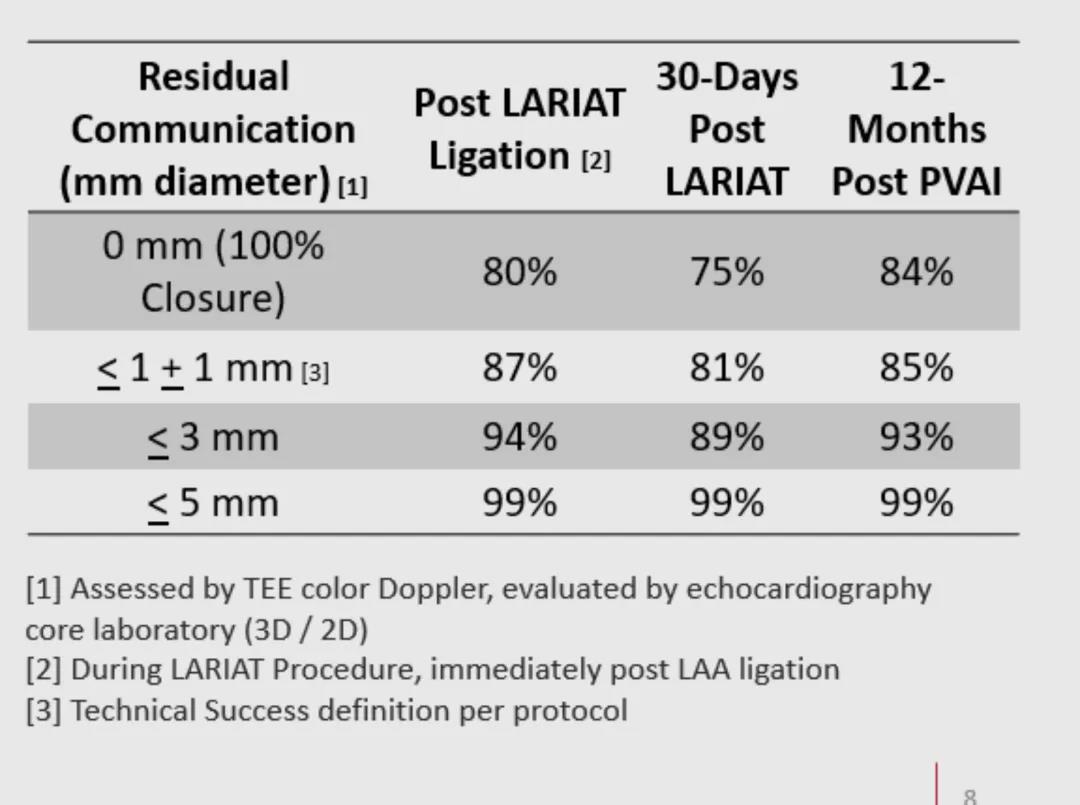
PVAI术后12个月LARIAT的LAA闭合率高(85 - 99%)(表3)。
表3: 技术成功指标
3、主要疗效终点
LARIAT + PVAI组PVAI后12个月无AA发生率为64.3%,仅PVAI组为59.9%,差异为4.3%;[95% Bayesian CI:-4.2,13.2],Bayesian后验概率= 0.835小于0.977(>0.977表示主要疗效终点成功),两组受试者的主要疗效终点并无明显差异(图2)。
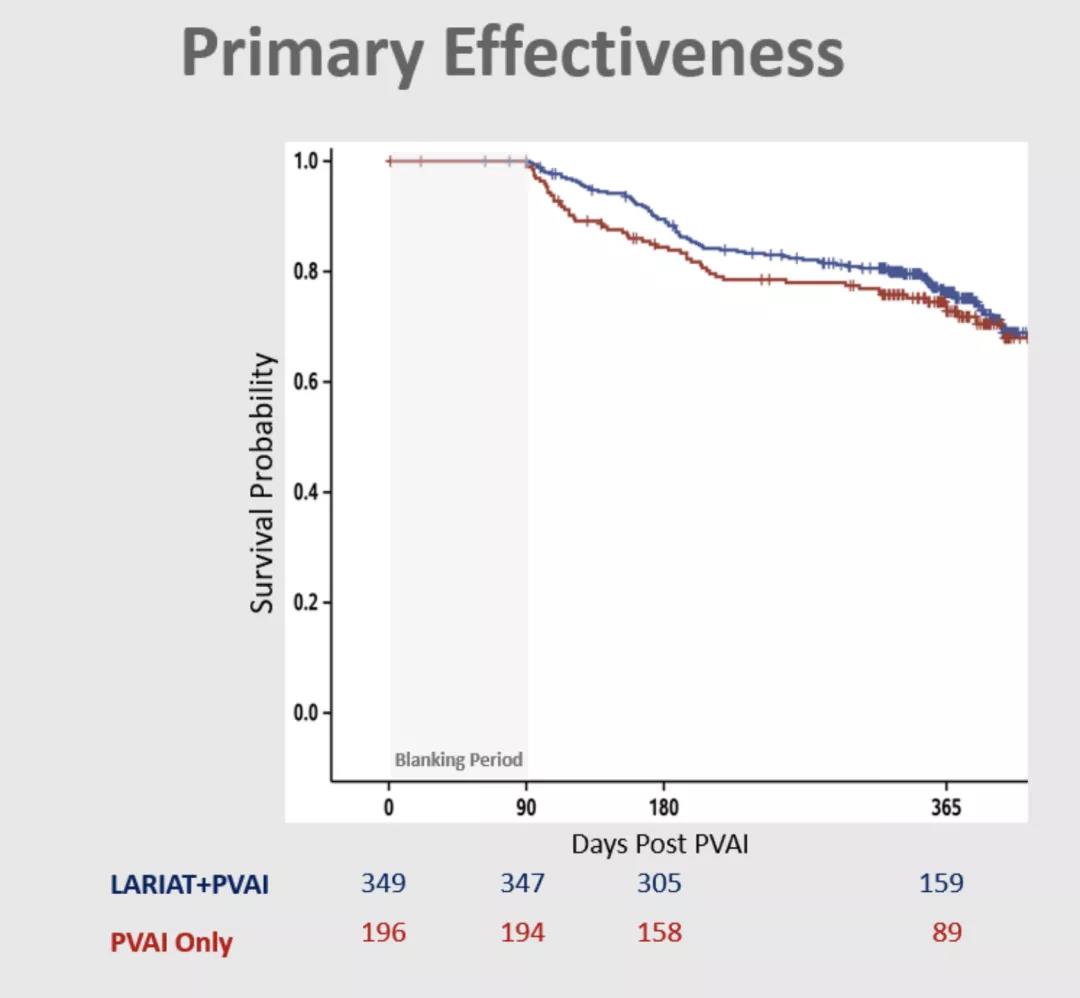
图2: 主要疗效终点
4、亚组分析
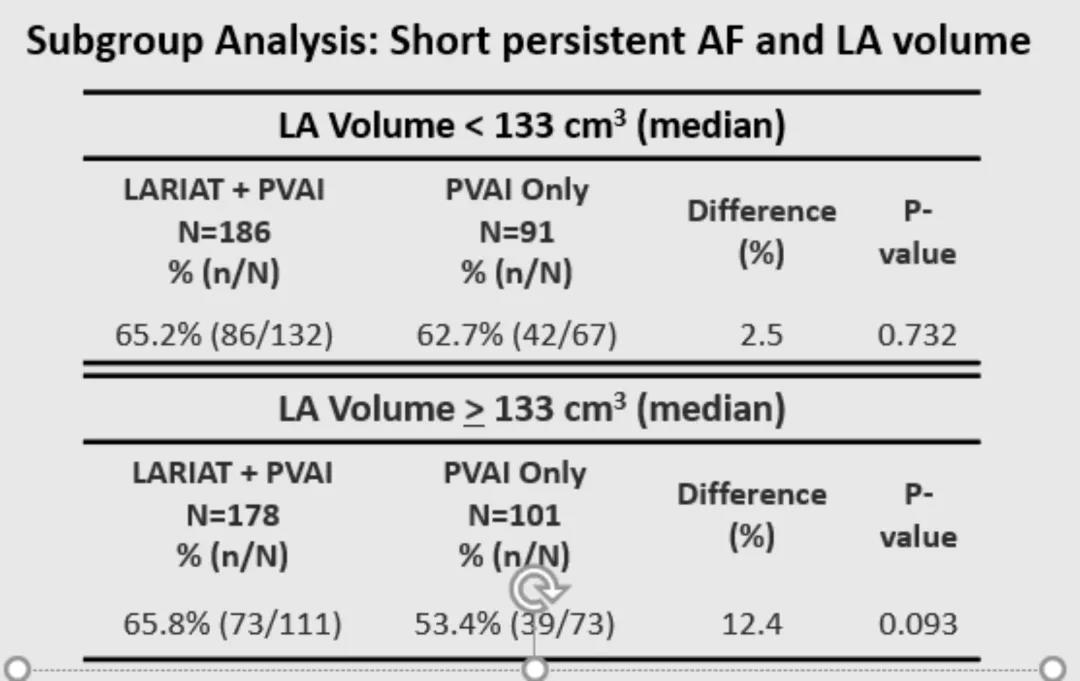
预先指定的亚组分析包括对按不同基线AF持续时间及LA体积分组的受试者的主要疗效终点差异进行分析。早期持续性AF亚组(Early Persistent)无AA受试者LARIAT + PVAI组66% vs. PVAI组58.5%;7.5%的差异P-value = 0.084 [95% Bayesian CI:-0.022,0.174];后验概率= 0.931(表4);早期持续性AF亚组(Early Persistent)无AA且LA体积增加(>133 cm3)受试者 LARIAT + PVAI组为65.8%,而PVAI组为53.4%;12.4%的差异P-value = 0.093 [95% Bayesian CI:-0.021, 0.263];后验概率= 0.952(表5)。
表4:AF持续时间

表5: LA体积
研究结论
AHA 2021丨AMAZE
LARIAT装置可安全有效的结扎LAA,对于接受房颤消融治疗的持续性房颤患者,在减少房颤复发性心律失常方面,辅助LAA结扎并不优于单独肺静脉窦隔离;探索性分析表明,在早期持续性房颤和左心房体积较大的亚组中,LAA结扎辅助治疗有可能提供更好的节律控制。
专家点评
AHA 2021丨AMAZE
房颤患者PAVI术后高复发率和高卒中风险一直是房颤射频消融治疗的两大难题,LARIAT装置能够成功而稳定的缝合左心耳,其长期效果可与FDA批准的Watchman装置相媲美。现有数据表明,对于不能接受抗凝治疗的患者,使用LARIAT心外膜缝合术闭合LAA是降低卒中风险的一个很好的选择。随着经验和技术的改变,LARIAT手术的安全性也大大提高,目前已有第二代LARIAT系统,LARIAT+系统是根据最初系统的经验和教训开发的。新系统有一个更大的套圈,可容纳直径高达45 mm的LAA,有一个钢质编织轴,在轴内提供更大的径向强度,提供更好的扭矩力来克服心外膜鞘的影响,并且在LARIAT的远端放置了一个铂-铱“L”标记,以便在透视下容易检测到正确的方向。Bartus等人报告了这种新系统在58名患者中的初步经验,急诊成功率高,所有患者均急性完全闭合,没有设备或手术的相关并发症,只有一例晚期心包积液在30天后需要心包穿刺。随访1个月和3个月,左心耳闭合率分别为96.3%和92.3%,无大于3 mm的渗漏;12个月后没有卒中、栓塞事件或死亡。而LARIAT闭合LAA时,LAA电压出现的明显降低或完全消除,提示LARIAT缝合可能成为一种潜在的既可以实现电隔离,又可以预防卒中的治疗方案。AMAZE研究首次揭示了LARIAT缝合辅助PAVI术对预防房颤复发的安全性和疗效方面的影响,虽然在减少房颤复发性心律失常方面,LARIAT辅助LAA结扎并不优于单独静脉窦隔离,但是其稳定的左心耳隔离成功率以及在早期持续性房颤和左心房体积较大的亚组中,LAA结扎辅助治疗表现出来的更好的节律控制都值得让我们对LARIAT保持更大的期待。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#静脉#
73
#AZ#
65
#AHA#
80
#肺静脉隔离#
55
#左心耳#
96