Front Oncol:局部复发乳腺癌患者的危险因素以及手术治疗效果
2021-10-15 yd2015 MedSci原创
研究表明,在近代的乳腺癌治疗中,LRR率相对较低。肿瘤大小和淋巴结状态与LRR的风险相关,对选择的LRR患者进行挽救性手术取得了良好的结果。
乳腺癌是世界范围内最常见的癌症,也是女性癌症死亡的主要原因。随着对肿瘤生物学行为的更好理解,筛查技术的创新,以及综合多学科治疗策略的发展,更多的乳腺癌可以在早期诊断出来。小范围手术,例如,在某些选择的患者中,保乳手术(BCS)术后放射治疗和前哨淋巴结检测,在生存方面等同于乳房切除术和腋窝淋巴结清扫(ALND),而且并发症更少。局部复发(LRR)是乳腺癌临床相关的、主要的治疗失败模式。LRR模式因初次手术入路而异,主要累及乳房切除术后胸壁复发、BCS后残留乳房或区域淋巴结(LNs)。近期,来自上海交通大学附属瑞金医院的团队开展了相关研究,旨在评估大型乳腺癌队列中LRR的风险和预后因素。相关结果发表在Frontiers in Oncology杂志上。
研究回顾性分析2009年1月至2018年3月在上海交通大学附属瑞金医院接受手术的早期乳腺癌患者。LRR定义为在同侧乳腺(IBTR)、胸壁或区域淋巴结复发且没有并发远处转移(DM)。比较两组患者的特点和生存率。
共有5202名患者纳入研究。中位年龄为55岁(范围:22-93岁)。浸润性导管癌患者4454例(85.6%),淋巴结阳性患者1723例(33.1%)。在3769例(72.5%)患者中检测出ER阳性,1181例(22.7%)HER2阳性。在局部和全身治疗方面,1597例(30.7%)患者接受了BCS治疗,其他患者初始手术接受了乳房切除术。2563例(49.3%)患者接受SLNB, 2598例(49.9%)患者接受ALND,其余41例(0.8%)患者未接受腋部手术。2539例患者接受了辅助治疗,其中86.4%的患者接受了BCS治疗,32.1%的患者接受了乳房切除术。
在中位47.0个月(范围:3.0-122.5)的随访后,352例(6.8%)患者出现首次复发,其中87例(1.7%)LRR和265例(5.1%)DM。整体人群的5年LRR估计为2.2%:BCS患者为3.3%,乳房切除术患者为1.7%。
多因素分析显示肿瘤大小(p<0.001),组织学分级(p<0.001),淋巴结状况(p <0.001),分子亚型(p = 0.005),乳房手术(p<0.001),腋窝手术(p<0.001),辅助化疗(p = 0.013)与首次复发事件独立相关。LRR组与无复发组比较,肿瘤大小>2.0 cm (OR = 2.13, 95% CI 1.31-3.48, p = 0.002), LNs阳性(OR = 3.24, 95% CI 1.75-6.02, p <0.001),初始BCS (OR = 3.04, 95% CI 1.73 5.33, p<0.001),未接受辅助化疗(OR = 2.48, 95% CI 1.37 4.50, p = 0.003)、未接受辅助放疗(OR = 1.91, 95% CI 1.07-3.42, p = 0.030)是LRR发生的独立危险因素。
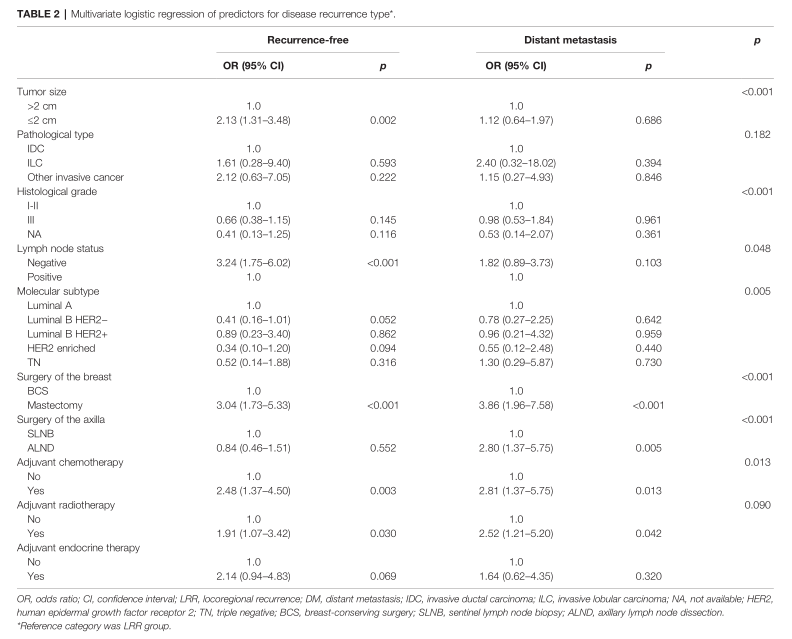
多因素分析复发相关因素
87例LRR患者中40例(46.0%)接受了进一步的挽救性手术。多因素分析显示原发肿瘤大小(p = 0.039)、腋部初始手术情况(p = 0.006)、LRR类型(p<0.001)是影响LRR手术选择的独立因素。原发性肿瘤较小、原发性SLNB和IBTR的患者接受手术治疗的可能性明显更高。局部LN复发患者接受手术的可能性低于仅IBTR患者(OR = 0.07, 95% CI 0.02 0.30, p<0.001);而胸壁复发和IBTR患者进行手术的可能性类似(OR = 0.36, 95% CI 0.09 1.47, p = 0.155)。
LRR患者、DM患者和无复发患者的5年OS率分别为80.7%、50.3%和98.8% (p <0.001)。
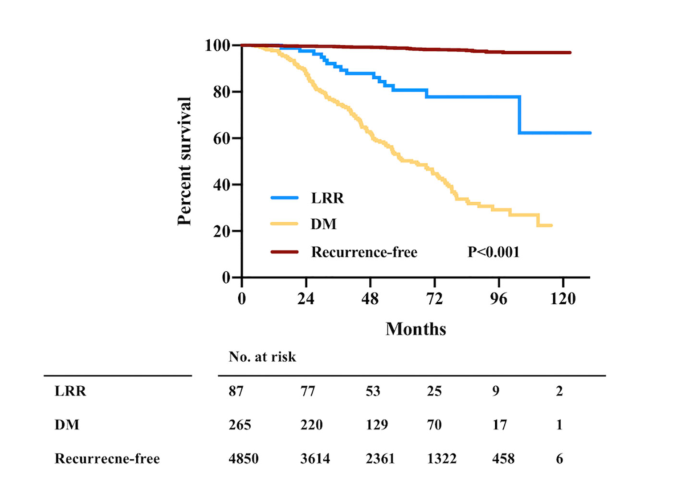
预后比较
复发后的中位随访时间为21.3个月(范围:1.0-77.5), 30例死亡病例。以LRR为首发事件的患者的PR-OS明显优于DM患者(3年PR-OS 75.0% vs. 37.1%;p<0.001)。87例LRR患者中,IBTR、胸壁复发、LN复发分别为26、27和34例。3年PR-OS分别为90.9%、77.3%和60.3% (p = 0.132)。LRR后接受手术的患者3年PR-OS估计为94.7%,显著高于未接受手术的患者(60.7%,p = 0.012)。
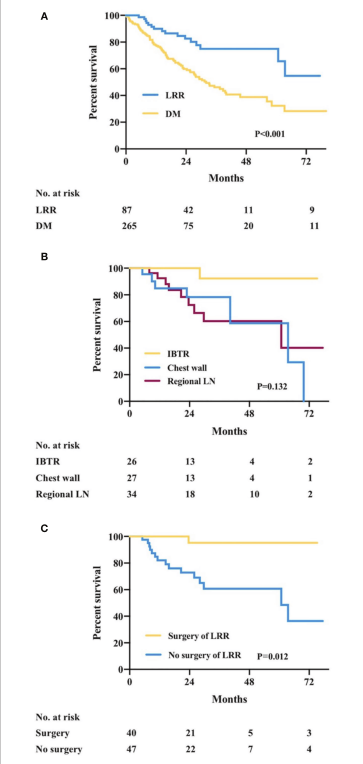
复发后预后比较
多因素分析显示,ER阳性(HR = 0.33, 95% CI 0.12 0.91, p = 0.033)和LRR挽救性手术(HR = 0.11, 95% CI 0.02 0.93, p = 0.043)与LRR患者PR-OS改善独立相关。
综上,研究表明,在近代的乳腺癌治疗中,LRR率相对较低。肿瘤大小和淋巴结状态与LRR的风险相关,对选择的LRR患者进行挽救性手术取得了良好的结果。
原始出处:
Huang J, Tong Y, Chen X and Shen K (2021)Prognostic Factors and Surgery for Breast Cancer Patients With Locoregional Recurrence: An Analysis of 5,202 Consecutive Patients. Front. Oncol. 11:763119. doi: 10.3389/fonc.2021.763119
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#治疗效果#
86
#Oncol#
84
#局部复发#
102
#手术治疗#
89
#局部#
90
#乳腺癌患者#
70