右心腔声学造影及肺动脉造影诊断肺动静脉瘘1例
2020-01-13 周宝风 翟亚楠 陶新曹 中日友好医院学报
患者女性,26岁,无明显诱因出现剧烈胸痛半日,于2017年10月24日来我院就诊。半日前患者出现胸痛,以右侧季肋区为重,疼痛剧烈,无放射性,呈持续性,与呼吸无关,后出现晕厥,约1min;无明显咳嗽、咳痰;无发热、咯血,痰中带血丝,夜间阵发呼吸困难;双下肢水肿,眼睑水肿、尿少。
患者女性,26岁,无明显诱因出现剧烈胸痛半日,于2017年10月24日来我院就诊。半日前患者出现胸痛,以右侧季肋区为重,疼痛剧烈,无放射性,呈持续性,与呼吸无关,后出现晕厥,约1min;无明显咳嗽、咳痰;无发热、咯血,痰中带血丝,夜间阵发呼吸困难;双下肢水肿,眼睑水肿、尿少。
急诊胸部CT示右侧胸腔积液、右肺膨胀不全、右肺中叶内侧段肿块,诊断为“胸腔积液、右肺占位”,为进一步诊治收入院。入院后行胸腔闭式引流术,引流暗红色胸水500ml,胸痛症状减轻。胸水病理回示:满视野红细胞,未见癌细胞。体温36.5℃,心率70次/min,血压100/60mmHg。WBC12.11×109/L,HGB107g/l,ESR13mm/h,凝血六项、肿瘤标志物、肿瘤组合、血氧饱和度、贫血三项正常。发育正常,口唇无紫绀、心界不大、心音有力、律齐。胸廓无畸形,呼吸运动右侧减弱,右侧肋间隙增宽。右下肺叩诊浊音,左肺呼吸音清晰,未闻及干湿啰音,右下肺呼吸音消失。超声心动图检查:各房室大小正常,心脏结构及功能未见异常。
2017年11月1日行右心腔声学造影(图1、2):经左肘静脉注右心声学对比剂(0.9%生理盐水9ml+1ml空气混匀后立即注射),心尖四腔心切面右心房右心室顺序充填较好,5个心动周期后,左心房、左心室可见中量(约11~30个微泡)对比剂气泡回声,持续时间较长。
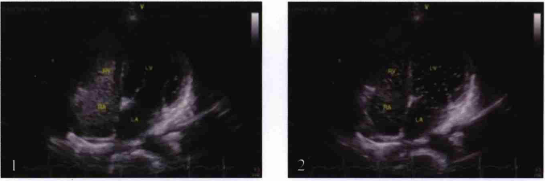
图1,2 显示右心房、右心室充盈后,5个心动周期后左心房、左心室出现对比机的过程(RA:右房;RV:右室;LA:左房;LV:左室)
右心腔声学造影提示:肺循环水平肺动静脉分流,肺动静脉瘘(pulmonary arteriovenous fistula,PAVF)不除外。
11月1日进一步行胸部增强CT(图3):各房室大小正常,主肺动脉不宽。右肺中叶可见明显强化不规则结节灶,边缘可见不规则充盈缺损,右侧胸腔积液,右下肺膨胀不张,右肺中叶动静脉畸形(arteriovenous malformation,AVM)并瘤内附壁血栓形成。11月9日局麻下行肺动脉造影及右侧肺动脉血管畸形栓塞术。造影可见右肺中叶内侧段肺动静脉异常血管及分流(图4)。应用COOK微弹簧圈行异常血管栓塞术,手术过程顺利,之后造影见血管畸形及分流消失(图5)。

图3 右肺中叶可见明显不规则结节灶(箭头所示)
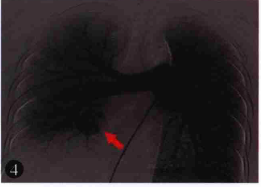
图4 术前右肺动脉中叶内侧支(RPA5)动静脉畸形(箭头所示)
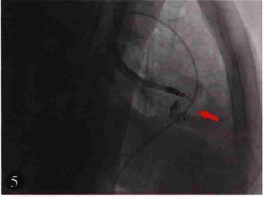
图5 术中应用COOK微弹簧圈行右肺动脉中叶内侧支(RPA5)栓塞术(箭头所示)
术后患者症状明显好转,无胸痛,间断发热,最高达37.6℃(考虑为胸腔积液吸收有关)。术后复查胸部增强CT:右肺中叶内侧段AVM术后,未见充盈缺损,瘤体闭塞(图6)。
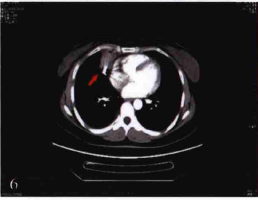
图6 右肺中叶内侧段AVM术后,瘤体闭塞(箭头所示)
讨论
PAVF在临床上较少见,其症状缺乏特异性,相当多的患者以并发症为首要甚至唯一的症状。本例患者为囊状肺动静脉瘘,因分流量较小,故患者未出现低氧血症。但患者出现阵发呼吸困难,胸部CT提示右侧胸腔积液、右肺中叶内侧段肿块,行胸腔闭式引流出暗红色胸水,胸水病理满视野红细胞,提示有血性液体渗出。行右心腔声学造影及胸部增强CT,提示为右肺动静脉畸形。随后行肺动脉造影及右侧肺动脉血管畸形栓塞术,证实了上述诊断。
本例患者因右心腔声学造影提示性的诊断,才避免了对右肺内侧肿块穿刺活检的风险。PAVF也称为肺动静脉畸形,指肺动脉与肺静脉之间存在异常血管,直接连接形成肺血管畸形,部分肺动脉血液可通过瘘管经肺静脉直接回流到左心房。大多数PAVF系先天性肺血管畸形,是肺部毛细血管发育畸形所致。极少数系肺部炎症、肿瘤、寄生虫、外伤等后天性病变侵犯肺血管,在肺动静脉之间形成瘘管所致。临床分为2种类型:Ⅰ型为弥漫性肺小动静脉畸形;Ⅱ型为囊状PAVF。
本病较少见,多见于青年,分流小者可无症状,分流大者由于PAVF造成肺动脉血液未经氧合,直接进入肺静脉致血氧饱和度降低,可出现心悸、呼吸困难、胸痛、咯血、紫绀,甚至晕厥、缺氧性发作,患者还可出现杵状指(趾)。随着病程延长,动静脉瘘数目和血管扩张程度有增加的趋势。虽然呼吸困难是最常见的症状,但大多数患者就医的直接原因通常是咯血。此外,因肺体循环直接相通,易致感染性心内膜炎、脑脓肿等并发症。对本病早期正确诊断具有重要临床意义,不但能早期治疗,提高患者生存质量,甚至能挽救生命。
长期以来,肺血管造影是诊断PAVF的“金标准”,但这是一种有创性检查,实际能完成此项检查的患者很少,且对于微小的多发弥漫性PAVF常常不能显示;多层螺旋CT可从各个角度较清晰地显示肺血管的解剖和病变特征,在诊断中发挥着重要作用,但其价格昂贵,少数患者可出现造影剂过敏或其他不适,不易做为常规检查。右心腔声学造影检查虽然不能确定肺静脉瘘的数目及具体位置,但是一种无创诊断本病的方法。它通过外周静脉注入造影剂(0.9%生理盐水9ml+1ml空气混匀)致右心显影。对于无右向左分流的患者,造影剂微泡很快出现在右房,微泡在通过肺毛细血管床时被滤过而消失,因此整个左心系统看不见造影剂微泡。若存在心房水平的右向左分流,气泡在右房出现的同时,1~3个心动周期之内进入左房。
而对于PAVF的患者,由于存在肺内右向左分流,造影剂出现于右心后要延迟4~5个心动周期,气泡才能进入左房。如果气泡可直接通过肺静脉进入左房,则提示存在肺动静脉解剖部位的异常。由于本病是由动静脉系统“短路”引起,所以常规超声心动图心脏各房、室腔内径大致正常,各心瓣膜形态、活动正常,心内无分流。对于高度怀疑本病的患者,可首做右心腔声学造影检查鉴别。
目前治疗PAVF主要方法有手术治疗、经导管栓塞治疗(transcatheter embolotheapy,TCE)及药物治疗,其中前两者是目前行之有效的方法:(1)手术治疗是根治性的治疗措施。方法包括结扎、肺段切除、肺叶、局部或全肺切除等。手术时应注意PAVF往往位于脏层胸膜下,且瘘周组织非常薄,很容易破裂出血,必须仔细解剖,细心操作。严重的弥漫性PAVF是双侧肺移植的适应证。(2)TCE是目前治疗PAVF的首选方法,具有相对安全、高效、经济、耐受性好、恢复快特点,可最大限度的保存肺组织,并易于多次重复操作。但有5%~10%的PAVF可能出现瘘管再通,需要定期密切随访,右心声学造影不仅可以明确诊断方向,而且可以快速无创评价PAVFS术后即刻及远期效果。
原始出处:
周宝风,翟亚楠,陶新曹,刘敏.右心腔声学造影及肺动脉造影诊断肺动静脉瘘1例[J].中日友好医院学报,2019,33(01):58-59+66.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#静脉#
43
#右心腔#
63
#声学造影#
89
#动静脉瘘#
119
#造影#
65