Neurology:千万别误诊为皮层静脉血栓,因为治疗完全不同
2018-02-13 杨中华 脑血管病及重症文献导读
66岁,女性,主因意识丧失后右下肢抖动到急诊室就诊。
66岁,女性,主因意识丧失后右下肢抖动到急诊室就诊。
既往:2周前头外伤史。
平扫头CT未见特异性改变。第二天脑增强MRI显示左侧中央后回异常信号(下图A-C)。
下图A,flari显示病灶高信号;图B,未见强化;图C,GRE显示含铁血黄素沉积:
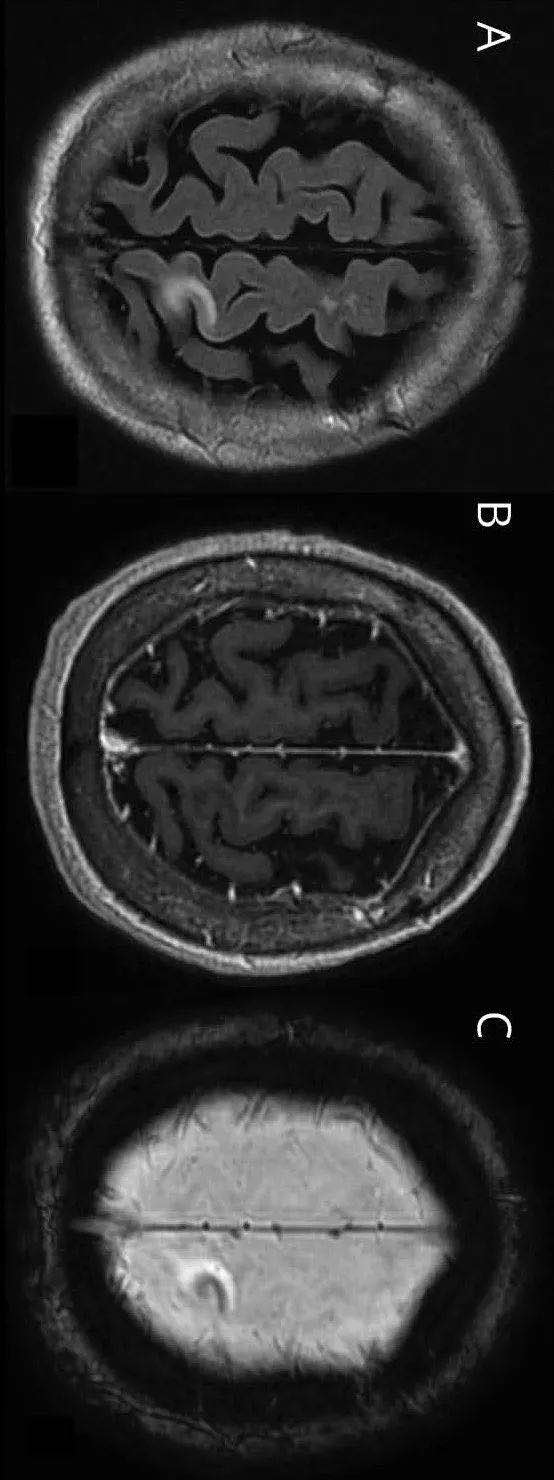
第四天右侧肢体无力加重。复查脑MRI显示左侧中央后回病灶扩大,伴占位效应、水肿以及可疑层状坏死。由于病情加重,患者被转到上级医院继续治疗。转院后复查脑MRI显示水肿加重,微出血,以及皮层病灶强化(下图D-F)。
下图D,Flair显示病灶扩大;图E,可见新发强化;图F,SWI显示含铁血黄素沉积:

由于不排除血管炎或皮层静脉血栓,随后进行了血管造影检查。DSA发现动静脉短路(arteriovenous shunt):脑膜中动脉额支直接汇入硬膜下静脉。静脉增粗(动脉直径的2倍)引流到上矢状窦(下图)。静脉异常与脑实质病变相符。
下图,左侧颈动脉造影显示脑膜中动脉额支直接汇入硬膜下静脉(箭头):
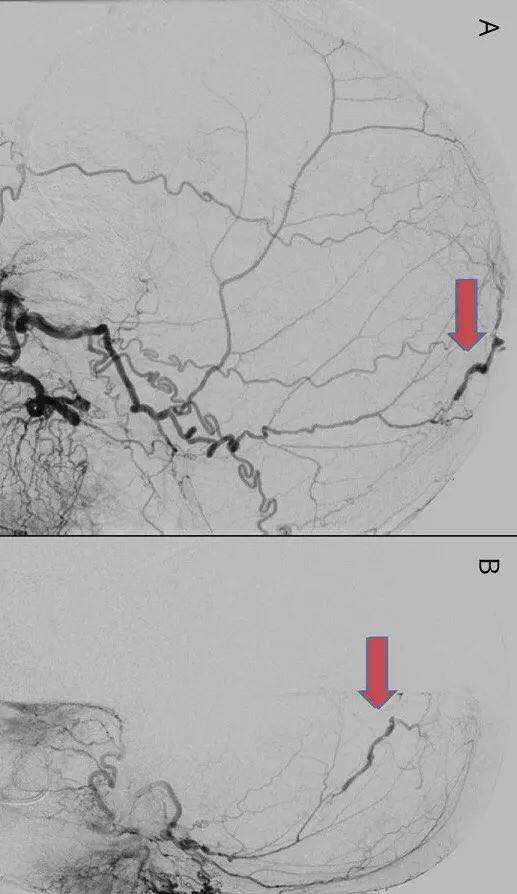
由于入路问题,无法进行介入栓塞术。随后神经外科颅骨切除术发现硬膜内静脉与皮层静脉相通,术中电凝。皮层静脉变蓝,无搏动,提示皮层静脉供血仅来自动静脉瘘。
手术后,患者右侧无力迅速好转。几个月后,患者能够骑自行车,跑步,残留右足稍无力。
最终诊断为硬脑膜动静脉瘘,患者的头部创伤可能是瘘的病因。
原始出处:
Béatrice Deschênes St-Pierre, et al. Clinical Reasoning: A 66-year-old woman with seizures and progressive right-sided weakness. Neurology. Jan 29, 2018.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#静脉血#
64
#静脉#
59
#Neurol#
61
学习谢谢分享
94