Eur Heart J-Card Img:慢性阻塞性肺疾病急性心肌梗死后左室整体纵向应变与长期预后!
2018-03-01 xing.T MedSci原创
由此可见,左心室GLS受损与伴有COPD的STEMI患者糟糕的长期生存率独立相关,并会增加LVEF的预测价值。
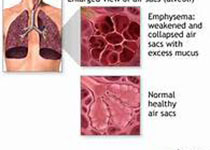
左心室(LV)收缩功能是ST段抬高型心肌梗死(STEMI)患者的一个已知预后因素。近日,心血管领域权威杂志Eur Heart J-Card Img上发表了一篇研究文章,研究人员旨在评价左心室整体纵向应变(GLS)在慢性阻塞性肺疾病(COPD)患者发生STEMI后的预后价值。
研究人员对一百四十三名伴有COPD的STEMI患者(平均年龄为70±11 岁,71%为男性)进行了回顾性分析。入院后48 小时内受试者通过经胸超声心动图测定了左室射血分数(LVEF)和左室GLS。患者随访至全因死亡和全因死亡以及心力衰竭住院的联合终点发生。
中位随访68(四分位距为38.5-99)个月,66例(46%)患者死亡,70例(49%)患者发生复合终点。平均左室GLS为-14.4%。LV的GLS>-14.4%的患者表现出较高的全因死亡(在随访1年、2年和5 年分别为19%、26%和44% vs. 7%、8%和18%;P=0.004 )和复合终点(26%、34%和50% vs. 8%、10%和20%;P=0.001)累积发生率,相比于左室GLS≤-14.4%的患者。在多变量分析中,左室GLS>-14.4%与增加的全因死亡和复合终点独立相关[风险比(HR)为2.07;P=0.02 和HR为2.20;P=0.01]。
由此可见,左心室GLS受损与伴有COPD的STEMI患者糟糕的长期生存率独立相关,并会增加LVEF的预测价值。
原始出处:
Laurien Goedemans,et al. Left ventricular global longitudinal strain and long-term prognosis in patients with chronic obstructive pulmonary disease after acute myocardial infarction. Eur Heart J-Card Img. 2018. https://doi.org/10.1093/ehjci/jey028
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#阻塞#
65
#长期预后#
74
#ART#
59
#HEART#
62