TOMY自锁矫治技术对非拔牙矫治前牙反牙合伴中度拥挤患者矫治效果1例报告并文献复习
2018-04-28 于彦君 胡荣荣 徐山山 吉林大学学报:医学版
患者,男性,22岁,因牙齿排列不齐于2014年4月就诊于吉林大学口腔医院正畸科。
【一般资料】
患者,男性,22岁
【主诉】
因牙齿排列不齐于2014年4月就诊于吉林大学口腔医院正畸科。
【现病史】
从正面观察,患者面部左右不对称,颏部左偏;从侧面观察,患者为直面型,下颌略前突(图1)。
【体格检查】
患者为恒牙列,右侧磨牙中性牙合关系,左侧磨牙近中牙合关系;13-23/43-33反牙合,反覆牙合浅;13唇向低位、完全位于牙弓唇侧;上牙弓II度拥挤,下牙弓I度拥挤;上牙列中线右偏约1.0mm,下牙列中线左偏约2.5mm(图1)。患者双侧颞下颌关节未见明显弹响及压痛,开口度、开口型未见明显异常。

图1 患者治疗前面像(A~C)和口内像(D~H)
【辅助检查】
曲面断层片(图2)显示:38水平阻生,48近中倾斜阻生,28牙胚发育过小,双侧下颌升支长度不对称,右侧略长。根据临床检查、模型分析及头颅定位侧位片测量结果,
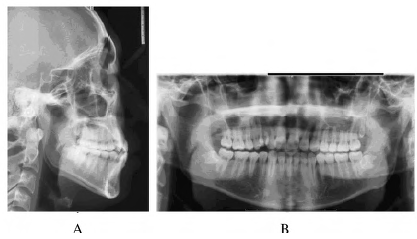
图2 患者治疗前X线片
【初步诊断】
该患者诊断为安氏I类亚类错牙合、毛氏H1+I1类错牙合、高角、面部不对称。
【治疗】
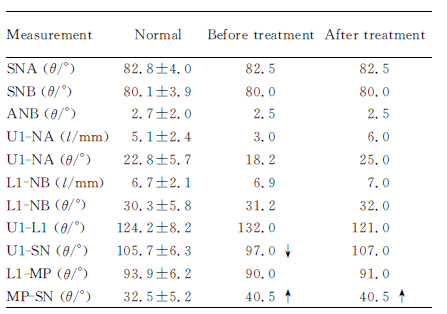
初诊时全口粘接TOMY金属自锁托槽,上下颌扎入0.014英寸含铜镍钛丝,开始排齐整平,并逐步更换热激活弓丝。4个月后,下颌扎入0.018×0.025英寸HANT,上颌仍为0.014英寸含铜镍钛丝,此时开始配合13、43、44垂直轻力弹性牵引(2盎司),同时建议患者加强闭唇训练,避免上前牙在排齐过程中过度唇倾。当上下颌牙列排齐整平后,上下颌逐渐更换0.018×0.025英寸HANT、0.018X0.025英寸SS,同时配合双侧尖牙区颌间垂直牵引,改善咬合关系,精细调整。图3为患者治疗6及13个月后口内像。19个月后去除口内上下颌固定矫治器,结束固定治疗,开始进入保持阶段。1.3数据整理与分析X线头颅定位侧位片测量标志点:蝶鞛点(S),蝶鞛影像的中心;鼻根点(N),鼻额缝的最前端;上牙槽座点(A),前鼻棘与上牙槽缘点间的骨部最凹点;下牙槽座点(B),下牙槽突缘点与颏前点间的骨部最凹点;上中切牙点(U1),上中切牙切缘的最前点;下中切牙点(L1),下中切牙切缘的最前点。测量项目:SNA角,蝶鞛中心、鼻根点、上齿槽座点连线所构成的角;SNB角,蝶鞍中心、鼻根点、下齿槽座点连线所构成的角;ANB角,上齿槽座点、鼻根点、下齿槽座点连线所构成的角;U1-NA角,上中切牙长轴与鼻根点-上牙槽座点连线交角;U1-NA距:上中切牙切缘至鼻根点-上牙槽座点连线的垂直距离;L1-NB角,下中切牙长轴与鼻根点-下牙槽座点连线交角;L1-NB距:下中切牙切缘至鼻根点-下牙槽座点连线的垂直距离;上下中切牙角(U1-L1),上中切牙长轴与下中切牙长轴的交角;上中切牙-前颅底平面角(U1-SN),上中切牙长轴与前颅底平面(SN)相交的下内角;下中切牙-下颌平面角(L1-MP),下中切牙长轴与下颌平面相交的上内角;下颌平面角(MP-SN),下颌平面与前颅底平面的交角。牙弓宽度包括牙弓前段宽度(anterior):左右侧尖牙牙尖间宽度;牙弓中段宽度(middle):左右侧第一前磨牙中央窝间宽度;牙弓后段宽度(posterior):左右侧第一磨牙中央窝间宽度。牙槽骨宽度(alveolarbonewidth)即左右侧第一前磨牙牙槽骨最凸点间的距离。基骨弓宽度(basalbonewidth)即左右侧第一前磨牙颊侧移行皱襞处牙槽骨最凹点间的距离。牙弓长度的测量方法是以左右侧第二恒磨牙远中接触点间连线为底线,由中切牙近中接触点向底线所作的垂线为牙弓总长度(total)。其中切牙近中接触点至尖牙连线的垂距为牙弓前段长度(anterior);尖牙连线至第_磨牙近中接触点连线的垂距为牙弓中段长度(middle);第一磨牙近中面连线至第二磨牙远中面连线间垂距为牙弓后段长度(posterior)。分别测量患者矫治前后X线头颅定位侧位片,在模型上测量矫治前后牙弓各段长度和宽度,牙槽骨宽度及基骨弓宽度,所有测量均由同一名研究者完成,测量3次,其值以平均数形式表示,对其治疗前后的各个指标测量值进行比较。2.结果2.1外部特征表现矫治后患者上下颌牙列排齐整平,前牙覆牙合覆盖正常,中线居中,上下中线一致,双侧尖牙、磨牙均达到中性牙合关系,上下牙弓宽度协调,面部左右基本对称协调(图4)。曲面断层片(图5)见:所有牙根平行,未见明显吸收现象,38水平阻生、48近中倾斜阻生,建议患者拔除,但患者拒绝拔牙。2.2定量指标矫正前后X线头颅定位侧位片测量值比较结果示:SNA、SNB和ANB无明显变化,上前牙唇倾度增加10°达到正常值,上下中切牙角减小11°。矫治前后模型测量结果显示:与矫治前相比,矫治后上下颌牙弓宽度都有增加,上牙弓宽度的增加主要表现在中段前磨牙区,增加了5.04mm,而下牙弓宽度的增加主要表现在后段磨牙区,增加了3.04mm;对于牙槽骨宽度和基骨弓宽度,治疗后均有所增加;治疗后,上下颌牙弓长度也有所增加,尤其上颌前段牙弓长度增加最为明显,增加了305mm。
图3 患者治疗6(A~C)和13(D~F)个月后口内像
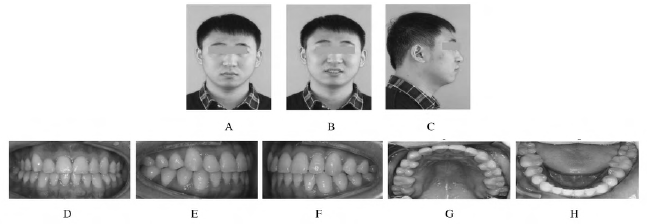
图4 患者治疗后面像(A~C)和口内像(D~H)
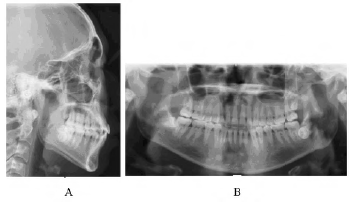
图5 患者治疗后X线片
原始出处:
于彦君, 胡荣荣, 徐山山,等. TOMY自锁矫治技术对非拔牙矫治前牙反伴中度拥挤患者矫治效果1例报告并文献复习[J]. 吉林大学学报:医学版, 2017, 43(2):416-421.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#前牙#
85
#拔牙#
66
学习了谢谢分享!!
61
好知识值得拥有的
156