肝纤四项的临床意义!一文读懂!
2015-12-21 佚名 医学之声
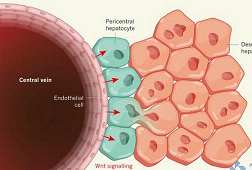
PCIII (III型前胶原) 反映肝内III型胶原合成,血清含量与肝纤程度一致,并与血清γ-球蛋白水平明显相关。PCIII与肝纤维化形成的活动程度密切相关,但无特异性,其它器官纤维化时,PCIII也升高。持续PCIII升高的慢活肝,提示病情可能会恶化并向肝硬变形成发展,而PCIII降至正常可预示病情缓解,说明PCIII 不仅在肝纤维化早期诊断上有价值,在慢性肝病的预后判断上也有意义。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











我想知道有没有什么肾脏纤维化的特异指标
157
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
135
有意思
156
赞一个
137
值得看,好好收藏
140
nice
101