J Clin Oncol:转移性胰腺癌的一线治疗该何去何从?
2021-07-22 MedSci原创 MedSci原创
对于使用 FOLFIRINOX诱导化疗4个月后病情得到控制的mPC患者,使用亚叶酸+氟尿嘧啶维持治疗似乎是可行和有效的
虽然医疗技术不断发展,但目前转移性胰腺癌 (mPC) 的预后仍然较差,5年生存率<5%。系统性化疗是mPC的标准疗法。PRODIGE 4—ACCORD 11试验证明,mPC患者采用氟尿嘧啶、亚叶酸、伊立替康和奥沙利铂 (FOLFIRINOX) 化疗6 个月的总生存率优于吉西他滨。但奥沙利铂相关的高限制性神经毒性使得我们需要在 mPC 患者中尝试奥沙利铂“用用停停”策略和序贯治疗策略。
这是一项II期研究,mPC患者被随机分组接受6个月的FOLFIRINOX(A组),4个月的FOLFIRINOX、继以亚叶酸+氟尿嘧啶维持治疗(B组),或每2个月交替使用吉西他滨和氟尿嘧啶、亚叶酸和伊立替康的序贯治疗(C组)。主要终点是6个月时的无进展生存率。
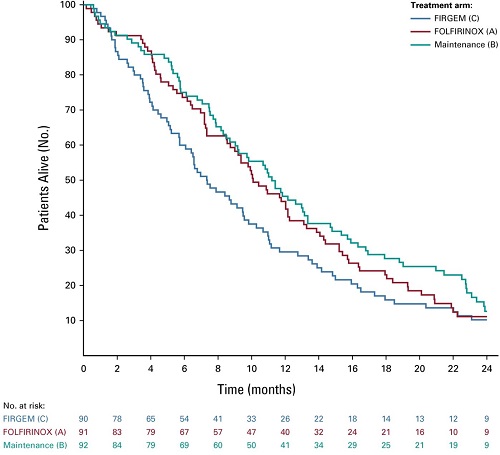
各治疗组患者的生存期
2015年1月-2016年11月,共招募了276位患者(平均63岁;范围 40-76岁):A组 91位、B组 92位、C组 90位。A组和B组的3/4级神经毒性的发生率分别是10.2%和19.8%。A组和B组奥沙利铂的接受剂量/目标剂量的中位数比率分别是83%和92%。A组、B组和C组的6个月无进展生存率分别为47.1%、42.9%和34.1%,中位总生存期分别为10.1个月、11.2个月和7.3个月。维持组的生活质量评分无恶化的中位生存期长于A组和C组(11.4个月 vs 7.2和7.5个月)。
不同治疗组生活质量评分不恶化的患者的生存期
综上所述,对于使用 FOLFIRINOX诱导化疗4个月后病情得到控制的mPC患者,使用亚叶酸+氟尿嘧啶维持治疗似乎是可行和有效的。维持治疗组的重度神经毒性发生率较高,可能是因为奥沙利铂的累积剂量较高。
原始出处:
Dahan et al. Randomized Phase II Trial Evaluating Two Sequential Treatments in First Line of Metastatic Pancreatic Cancer: Results of the PANOPTIMOX-PRODIGE 35 Trial. Journal of Clinical Oncology. July 21, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














感谢分享,很有用
65
#Oncol#
39
#转移性#
52
#转移性胰腺癌#
53
谢谢梅斯分享这么多精彩信息
75