病例分享: “微”“难”之处显身手:尼可地尔缓解难治性心绞痛两例
2017-11-18 佚名 国际循环
尼可地尔具有双重作用机制,一方面作为高选择性KATP通道开放剂,可舒张血管平滑肌、扩张微小冠状动脉、增加冠状动脉血流量,模拟缺血预适应,保护心肌;另一方面具有类硝酸酯作用,可扩张大冠状动脉、舒张容量血管、减少前负荷。
病例1
患者男性,63岁,主因“反复活动后胸闷、胸痛10年余”入院。
现病史
患者于10年多前开始出现劳累后胸闷、胸痛,位于心前区,性质隐痛,约巴掌大小,无明显放射痛,持续数分钟后可自行缓解,未行诊治。近2年来病情较前加重,夜间或晨起可出现,持续半小时。患者于2017-05-12外院行冠状动脉造影见多处临界病变,给予“阿司匹林0.1 g qd、瑞舒伐他汀10 mg qn、美托洛尔缓释片23.75 mg qd、单硝异山梨酯缓释片50 mg qd”治疗,病情未见缓解,遂来我院就诊。
体格检查
血压130/78 mm Hg,神志清楚,两肺呼吸音清,未闻及干湿啰音。心界未见扩大,心率77次/分,律齐,未及杂音。双下肢未见浮肿。
辅助检查
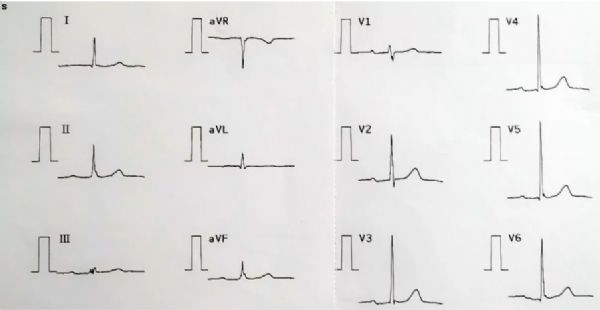
外院冠状动脉造影示,LM未见明显狭窄;LAD近段30%狭窄,中段50%狭窄,D1开口50%狭窄;LCX近段50%狭窄;RCA中段60%狭窄,后分叉前70%狭窄。入院心电图可见Ⅰ度房室传导阻滞(图1)。
图1. 心电图示Ⅰ度房室传导阻滞
初步诊断
冠心病 不稳定性冠心病
Ⅰ度房室传导阻滞
诊疗经过
患者冠状动脉存在多支病变,并可见多处临界病变,未行介入治疗。既往单纯药物治疗未能使其病情缓解,需复查冠状动脉造影并行FFR检查以明确冠状动脉病变是否为罪犯病变。冠状动脉造影(图2)结果显示:LM未见明显狭窄;LAD中段略显毛糙,可见20%~30%狭窄,D2分支开口约50%狭窄;LCX近段可见60%狭窄;RCA第2转折处约60%狭窄,后分叉前约70%狭窄。进一步评估LAD、LCX及RCA的FFR分别为0.88、0.94和0.92(图3)。




图2. 冠状动脉造影

图3. FFR测定
该患者临床症状支持存在心肌缺血,但冠状动脉造影及FFR检查无法确定罪犯血管,故无法实施进一步介入干预。此外,患者存在Ⅰ度房室传导阻滞,限制了足量β受体阻滞剂的安全应用,而现有长效硝酸酯类药物对胸痛症状控制效果欠佳。另外,患者病情特点高度提示存在冠状动脉微循环障碍或冠状动脉痉挛,故有必要调整药物治疗方案。遂将瑞舒伐他汀用量加倍,将美托洛尔改为地尔硫卓,单硝酸异山梨酯改为尼可地尔;后患者胸痛缓解,且出院前未再发作。
病例2
患者男性,66岁,主因“反复胸闷、胸痛半年余”入院。
现病史
患者于2016年12月开始出现反复胸闷、胸痛,以夜间至上午多见,活动后明显,位于心前区,每次持续5~10分钟,含服“复方丹参滴丸”可缓解。2017年3月及6月外院两度造影提示多处临界病变,给予“阿司匹林、氯吡格雷抗血小板聚集,瑞舒伐他汀调脂,单硝酸异山梨酯缓释片扩血管,美托洛尔及卡托普利降压”等治疗。但患者病情未见缓解,入院前一天早晨再发胸闷、大汗伴头晕、黑朦,遂来就诊。
既往史、个人史
高血压病史10余年,最高150/100 mm Hg,间断服药。长期烟酒史。
体格检查
血压118/82 mm Hg,神志清楚,两肺呼吸音清,未闻及干湿啰音。心界未见扩大,心率60次/分,律齐,未及杂音。双下肢未见浮肿。
辅助检查
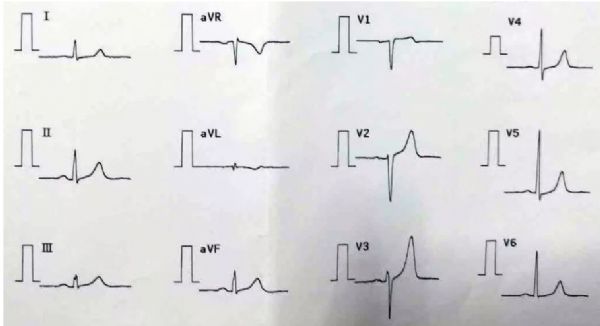
心电图未见异常(图4)。外院造影(图5)显示,LM未见明显狭窄;LAD近段30%~40%狭窄病变;LCX开口可见斑块,约50%狭窄,中远段60%狭窄病变1处;RCA中段约60%狭窄病变1处。动态心电图未见明显异常。
图4. 心电图未见异常
图5. 外院冠状动脉造影
初步诊断
冠心病 不稳定性冠心病
高血压病(2级 极高危)
诊疗经过
该患者存在冠状动脉多支病变,并可见多处临界病变,无法确认罪犯血管。既往单纯药物治疗并未缓解病情,而外院短时间内两度造影显然再次动员患者复查造影及FFR检查存在困难。患者临床症状支持存在心肌缺血,但冠状动脉造影无法确定罪犯血管并进一步介入干预。目前,患者冠心病二级预防药物使用相当全面,但现有药物治疗效果欠佳,包括长效硝酸酯类药物对其胸痛症状控制欠佳。此外,患者基础心率较慢限制了β受体阻滞剂的应用,而其胸痛夜间频繁发作符合冠状动脉痉挛导致缺血发作的特点,也是β受体阻滞剂应用的禁忌证。遂调整原有治疗方案,将美托洛尔换为地尔硫卓,将单硝酸异山梨酯换为尼可地尔;后患者胸痛缓解,出院前未再发作。
诊疗体会
研究发现,冠状动脉造影仅可检测到5%的冠状动脉树,95%的冠状动脉微循环无法显现。临床实践中,冠状动脉微血管病变(CMD)发生率较高,涉及患者人群广泛,且会增加不良事件风险,需予以关注和重视。冠状动脉微血管主要作用是为心肌供氧,通过代谢物质(如ATP)来调节,而ATP浓度又可调节ATP敏感性钾(KATP)通道活性。因此,KATP通道是调节微血管功能的重要环节,这也是尼可地尔用于治疗CMD的药理学基础。
尼可地尔具有双重作用机制,一方面作为高选择性KATP通道开放剂,可舒张血管平滑肌、扩张微小冠状动脉、增加冠状动脉血流量,模拟缺血预适应,保护心肌;另一方面具有类硝酸酯作用,可扩张大冠状动脉、舒张容量血管、减少前负荷。此外,研究发现,其还具有稳定斑块、改善内皮功能、抗炎/抗氧化应激、改善心脏交感神经活性及改善纤溶能力等作用。IONA研究显示,尼可地尔可显着降低稳定性心绞痛患者主要终点事件及心血管事件的发生风险;OACIS研究显示,尼可地尔可使PCI术后患者全因死亡风险显着降低43%。正因如此,尼可地尔受到2013欧洲稳定性冠心病指南、2013日本血管痉挛性心绞痛诊治指南及2011日本心肌梗死二级预防指南等多项指南的推荐。此外,与常用于改善胸痛症状的硝酸酯类药物相比,尼可地尔具有不良反应头痛发生率较低、对血压及心率无显着影响、无耐药性且作用可持续24小时等优势。
因此,临床实践中,对于症状典型且冠状动脉造影无法确认罪犯血管的心绞痛患者,需高度怀疑合并冠状动脉痉挛后微循环障碍。对于该类患者,尼可地尔具有独特优势,正所谓“微”(微循环障碍)“难”(难治性心绞痛)之处显身手!
评委点评
吴平生教授 南方医科大学南方医院
谢谢王主任带来了两个看起来很平常但实质上很经典的病例。两例都是60多岁男性,有轻度动脉粥样硬化但未达到需干预的程度,都是烟酒嗜好。大家不要小看烟酒嗜好,特别是吸烟,尼古丁对微循环的作用非常显着。指南特别强调危险因素控制,有烟酒嗜好一定要戒烟。另外,第1个病例的心电图,Ⅱ、Ⅲ、aVF导联都存在片段,这不是偶然,英文叫做fragment,翻译为碎片状的QS波。美国做过一项大型流行病学调查,发现这种患者其实发生过心肌梗死,这个现象还未引起大家高度重视,甚至指南都未提及,但临床上相当一部分患者其实发生过心肌梗死。排除束支传导阻滞后,如果出现这个问题,相当于发生过病理性Q波。右冠状动脉造影的后降支显示血流缓慢,所以他的QS波改变不是偶然的,造影剂能够慢慢过去,好像是慢血流。报告提到患者的前降支、右冠状动脉以及回旋支的FFR都是正常的。不同血管有不同的FFR,这个患者右冠状动脉FFR正常,但如果放在刚才血流慢的地方,肯定不正常。所以测量FFR要特别注意,看见了血流缓慢,应该在血流慢的地方测量,不同血管分支会影响FFR结果。这个病例很遗憾没有测IMR,FFR测量的是大血管,我们要看IMR即微循环阻力指数,相信患者IMR是有问题的。这个病例的治疗效果奇好,一定是解决了微循环问题。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#尼可地尔#
69
#难治性#
71
谢谢分享学习了非常好
93
厉害了我的哥
90
谢谢分享.学习了
83
学习一下谢谢
96