Nature:西班牙科学家发现肿瘤转移关键分子
2016-12-11 科学网 孙学军 科学网 孙学军
最新动物实验结果表明,癌细胞转移需要脂肪提高能源,这一发现给癌症转移的治疗带来新的策略。正常组织细胞一旦从原位脱离往往会启动自杀程序,不会带来对躯体的危害。癌细胞转移是癌症恶变的典型特征,也是患者死亡的关键。癌细胞转移对癌症细胞来说也是非常艰巨的任务,癌细胞转移过程包括从原位组织脱离,进入血液和淋巴等转移到身体其它部位,在完全不同的区域重新生长形成肿块。科学家一直在努力理解癌细胞转移的启动信号和具
最新动物实验结果表明,癌细胞转移需要脂肪提高能源,这一发现给癌症转移的治疗带来新的策略。
正常组织细胞一旦从原位脱离往往会启动自杀程序,不会带来对躯体的危害。癌细胞转移是癌症恶变的典型特征,也是患者死亡的关键。癌细胞转移对癌症细胞来说也是非常艰巨的任务,癌细胞转移过程包括从原位组织脱离,进入血液和淋巴等转移到身体其它部位,在完全不同的区域重新生长形成肿块。
科学家一直在努力理解癌细胞转移的启动信号和具体细节。2016年12月7日Nature发表的论文中确定了一类口腔肿瘤细胞如何实现转移的步骤,其中关键过程是这些肿瘤细胞转移需要的能量要依靠脂肪来提供。未参加该研究的休斯顿贝勒医学院癌症学家Xiang Zhang说,确定癌症转移过程,也就是癌症恶变过程的程序十分重要。
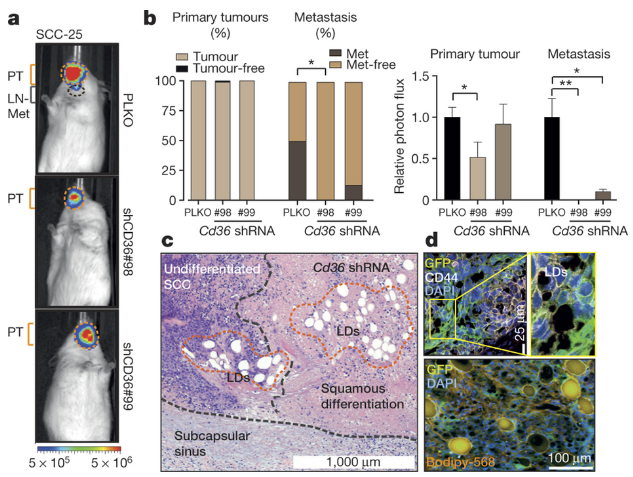
西班牙巴塞罗那理工学院Salvador Aznar Benitah等,通过对潜在具有转移能力的癌细胞进行研究,发现口腔癌症细胞中一些表达高水平CD36的细胞。CD36是一种脂肪酸受体,负责脂肪酸的识别和细胞跨膜转运,CD36能帮助肿瘤细胞从周围环境中摄取脂肪分子,这些脂肪分子成为这些细胞转移的能量来源。他们认为,肿瘤细胞转移需要大量额外能量,这些细胞能从环境中摄取脂肪使之具有了转移的能力。芝加哥大学妇科肿瘤学家Ernst Lengyel说:“转移需要大量的能量,癌细胞必须能够适应不断变化的环境,重新改变基因表达模式,建立滩头阵地并迅速开始增殖。”
Benitah等发现,小鼠体内转移的癌症细胞需要CD36的高表达,利用抗体阻断CD36与脂肪酸的结合就可以完全抑制肿瘤细胞的转移。但是这种抗体不会影响原位癌症的生长。
研究人员通过挖掘公共数据库,发现许多人类癌症如膀胱、肺癌、乳腺癌高表达CD36与恶劣预后存在相关关系,这提示这些癌症也存在类似的情况。Benitah团队正在努力开发CD36抗体药物,争取早日用于临床研究,初步估计4年后可以达到这一目标。Benitah指出,这是癌症细胞转移的针对性治疗策略,小鼠实验中这种抗体可以消除15%,剩余的转移肿瘤细胞也萎缩了80%以上。
团队也在思考另一个现象,给小鼠喂养高脂饮食导致肿瘤增长速度加快,有更多的淋巴结和肺转移现象。Benitah团队正在进行一项研究,计划招募1000人类癌症患者,通过分析这些患者血液中脂肪酸类型,寻找那些促进癌症转移的脂肪酸类型。根据现在的研究结果,建议人们控制脂肪类食物仍然为时过早,而且癌症患者往往需要更多热量维持生命,建议控制脂肪饮食可能适得其反。
原始出处:
Gloria Pascual,et al. Targeting metastasis-initiating cells through the fatty acid receptor CD36. Nature. 07 December 2016.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Nat#
41
#科学家发现#
36
#肿瘤转移#
77
#牙科#
59
顶
74
优秀
69