NSTE-ACS诊疗措施推陈出新
2011-09-06 MedSci原创 MedSci原创
此次新颁布的四大指南都历经了一年半以上的编写及3遍以上的审阅。除查阅大量文献,反映最新研究进展,指南制订者们还通过设计一系列简洁直观的图表或提供更具操作性的建议,提升指南的实用价值,并缩小与临床实践之间的差距。 一再更新,在变化中不断进步 诊断与危险分层更新点 证据级别提升:对疑似非ST段抬高急性冠脉综合征(NSTE-ACS)患者,应据病史、症状、体格检查、心电图和生物标志物结
此次新颁布的四大指南都历经了一年半以上的编写及3遍以上的审阅。除查阅大量文献,反映最新研究进展,指南制订者们还通过设计一系列简洁直观的图表或提供更具操作性的建议,提升指南的实用价值,并缩小与临床实践之间的差距。
一再更新,在变化中不断进步
诊断与危险分层更新点
证据级别提升:对疑似非ST段抬高急性冠脉综合征(NSTE-ACS)患者,应据病史、症状、体格检查、心电图和生物标志物结果进行诊断及短期缺血/出血危险分层(Ⅰ/A)。
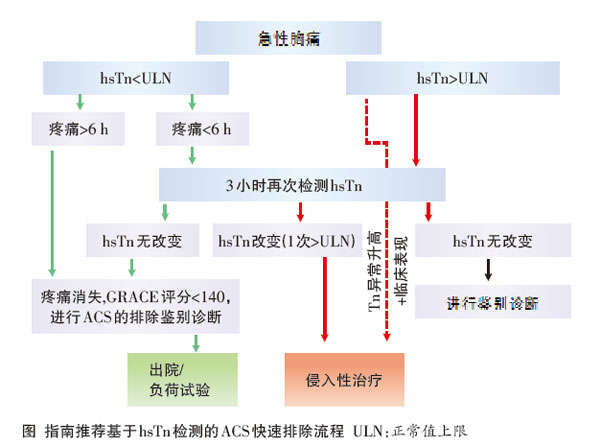
新增建议:①推荐对所有患者行超声心动图评估左室局部和总体功能,以诊断及鉴别诊断;②急性冠脉综合征(ACS)患者更适于收入胸痛中心或冠脉护理中心诊疗(Ⅰ/C);③建议应用风险评分(如GRACE和CRUSADE评分,后者首次获指南推荐,用于预测大出血风险)评估预后及出血风险(Ⅰ /B);④在可检测高敏肌钙蛋白(hsTn)情况下,推荐快速排除流程(Ⅰ/B,图);⑤当患者罹患冠心病的可能性低至中等,且肌钙蛋白和心电图结果不能确诊时,冠脉CT可被考虑作为侵入性造影替代手段用于排除ACS(Ⅱa/B)。
药物治疗更新点
口服抗血小板药:①对所有中、高危缺血事件患者(无论初始治疗策略如何,及是否接受了氯吡格雷预处理),推荐替卡格雷(负荷剂量180 mg,维持剂量90 mg/每天2次)(Ⅰ/B);②对首次接受P2Y12抑制剂的患者(尤其糖尿病患者),若冠脉解剖明确且拟行经皮冠状动脉介入术(PCI),则推荐普拉格雷(负荷剂量60 mg,维持剂量10 mg/d),除非患者具有威胁生命的高危出血风险或其他禁忌证(Ⅰ/B);③对有胃肠道出血或消化道溃疡病史,及多种其他危险因素(幽门螺杆菌感染、≥65岁、同时使用抗凝药或类固醇)的患者,推荐双重抗血小板治疗同时联合质子泵抑制剂(最好勿用奥美拉唑)(Ⅰ/A)。
糖蛋白(GP)Ⅱb/Ⅲa受体拮抗剂:在侵入性治疗中不推荐造影前常规使用此类药物(Ⅲ/A)。
抗凝治疗:①因在抗凝方面具有最佳疗效和安全性,磺达肝癸钠(2.5 mg/d,皮下注射)被推荐使用(Ⅰ/A);②对拟行紧急或早期侵入性治疗的患者,尤其出血风险高危者,比伐卢定暂时联合GPⅡb/Ⅲa受体拮抗剂可替代普通肝素(UFH)联合GPⅡb/Ⅲa受体拮抗剂的治疗方式(Ⅰ/B)。
侵入性评估及再血管化更新点
①侵入性策略(起病后72 h内)适用于症状反复出现或符合以下至少1项高危标准的患者:主要标准为肌钙蛋白水平升高或降低,以及ST段或T波出现动态改变;次要标准为糖尿病、肾功能不全[估计肾小球滤过率(eGFR)<60 ml/(min·1.73 m2)]、左心室功能减退(射血分数<40%)、早期梗死后心绞痛、近期行PCI治疗、既往行冠状动脉旁路移植术(CABG)及GRACE评分为中、高危(Ⅰ/A);②对于GRACE评分>140分或至少符合1项主要高危标准的患者,推荐其早期(<24 h)接受侵入性策略。
其他亮点
新指南将NSTE-ACS处理归为简单5步,即初始评估、明确诊断和风险评估、侵入性策略、再血管化治疗及出院和出院后,便于记忆;此外,还将疑似ACS患者治疗、PCI前抗栓治疗及出院措施等归纳为简要清单,以便医生检查治疗措施是否符合规范。
中国专家观点 四川省成都市第三人民医院 罗俊教授:

指南更新推动诊疗进步 近年来层出不穷的循证医学证据是促成NSTE-ACS指南不断更新的基础,通过11年间的数次修订,一些临床上的“灰色地带”得以被明确界定。指南更新对于当前所推崇的“循指南医学”而言意义重大,提供了与时俱进的规范化诊疗建议,有助于实现共性与个性治疗的相互统一与有机结合。
高敏肌钙蛋白和心脏超声促进早期诊断 新版指南推荐应用hsTn进行快速排除诊断,但这一检测技术尚未在国内广泛开展。由于诊断敏感性高,hsTn能早期发现并识别心肌损伤,从而早期诊断ACS。无独有偶,心脏超声也能通过早期发现心脏结构变化进行早期诊断,其价值也获得了新版指南的认可。上述两种诊断方法的临床应用可能促使NSTE-ACS诊疗策略向着早期诊断、上游甚至上上游治疗以及改善预后等方面发展,必将有助于减少严重并发症(如心源性休克)的发生。
危险分层利于医患双方 出血仍是NSTE-ACS患者面临的巨大挑战,新版指南首次推荐CRUSADE评分用于评估院内出血风险。从表面上看,危险分层增加了临床医生的工作负担,但医生每日接诊的ACS患者数量相对有限,且危险分层有利于制定更安全的诊疗策略,从而减少出血带来的医患矛盾,故这种医患双方均可获益的危险分层值得推广应用。
新型抗血小板药物临床获益更明确 PLATO和TRITON TIMI38研究证实了以替卡格雷和普拉格雷为代表的新型抗血小板药物的疗效及安全性,同时将上述两药“送入”了新版指南。基于新型抗血小板药物确实在疗效和安全性方面更胜一筹,出于减少缺血事件和改善预后的目的,使用这些药物或能给患者带来更多临床获益。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#诊疗措施#
73
#NST#
67
#NSTE-ACS#
67
#ACS#
78