Stroke:国药之光:天坛王拥军教授团队牵头TASTE试验3期结果为卒中患者带来新希望!
2021-02-22 MedSci原创 MedSci原创
急性卒中后48小时内给予依达拉奉右莰醇可以明显改善90天功能结局,尤其是女性患者获益更大。
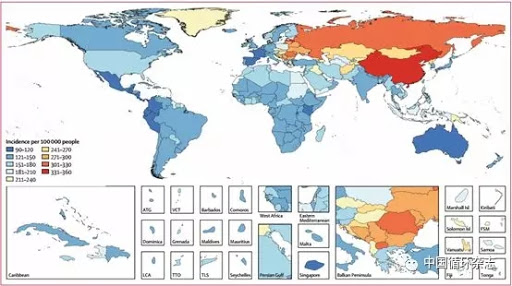
卒中,通常称为“中风”,是全球第二大死因,仅次于心血管疾病(CVD)。而中国是全球卒中负担最高的国家,终生风险高达39.3%。卒中具有发病率高、死亡率高、致残率高、复发率高“四高”的特点。目前,我国带病生存者高达1300万。
根据中国卒中学会联合中国疾病预防控制中心最新发布的《中国卒中报告2019》显示,仅2018年,我国因卒中死亡人数为157万人,约占全球卒中死亡人数的1/3,占居民总死亡率的22.3%,也就是说我国每五位死亡者中就有一人死于脑卒中。因此,卒中已成为我国成年人致死和致残的主要原因,同时也是过早死亡和疾病负担的首位原因。
急性缺血性脑卒中再灌注治疗的早期目标是恢复已缺血但尚未梗死脑区的血流。远期目标则是降低脑卒中相关致残率和死亡率,改善结局。目前,明确有效的再灌注治疗方案包括静脉用阿替普酶、静脉用替奈普酶和机械取栓。
然而,国内外有关神经保护剂的临床研究却始终没能得到令人满意的结果。依达拉奉是由日本田边三菱制药研发、生产和销售的一种抗氧化药物,用于清除自由基以治疗缺血性脑卒中等心脑血管疾病。依达拉奉于2001年4月在日本上市。
依达拉奉右莰醇是由两种活性成分组成的复方制剂。除外依达拉奉的抗氧化作用,右莰醇还可以抑制脑缺血再灌注导致的炎性细胞因子和致炎蛋白的表达,进而降低和改善AIS引发脑神经损伤。作为一种新型神经保护剂,早期的动物实验已经证明依达拉奉右莰醇具有抗氧化和抗炎的协同作用。
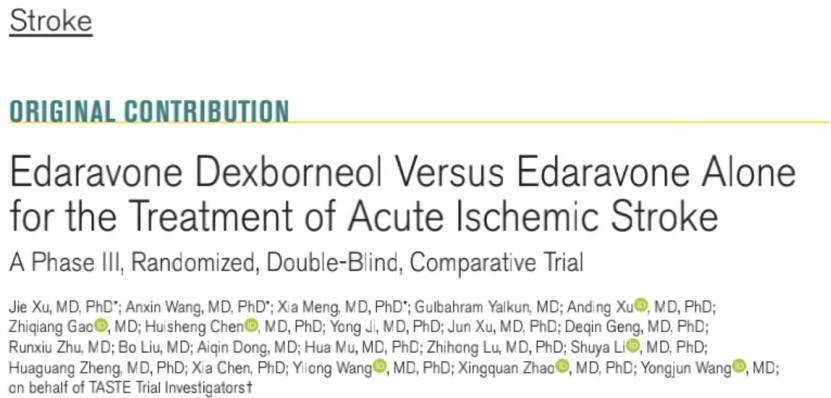
为此,北京天坛医院王拥军教授牵头,在中国48个医学中心开展了TASTE试验,以检测与单用依达拉奉相比,依达拉奉右莰醇对急性缺血性脑卒中(AIS)患者90天功能结局的影响。结果发表在美国卒中协会(ASA)旗下《卒中》(Stroke)杂志上。
该研究为多中心、随机、双盲、比较、III期临床试验。2015年5月至2016年12月期间,在中国48家医院同时开展。共纳入了1200名年龄35~80岁,NIHSS评分在4~24分之间,且在发病48小时内的急性卒中患者。
将患者以1:1的比例随机分为2个治疗组:14天输注依达拉奉右莰醇或依达拉奉注射液。主要终点是随机化后90天改良Rankin量表评分(mRankin)≤1的患者比例。
结果显示,两组分别有585人与580人入组。总的来说,与依达拉奉组相比,依达拉奉右莰醇组在卒中第90天出现良好功能结果(mRankin≤1)的患者比例明显更高(67.18% vs 58.97%),几率高42%。同时,预先指定的亚组分析表明,女性患者的获益约倍为男性患者的2倍(2.26 vs 1.14)。
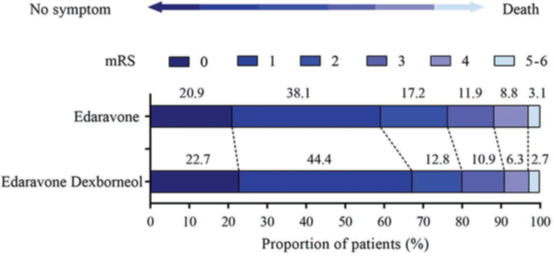
此外,在副作用方面,包括不良反应发生率(93.16% vs 93.95%)、严重不良反应发生率(9.02% vs 7.90%)、死亡人数(1.34% vs 1.68%),两组表现都没有显著差异。
综上,该研究表明,急性卒中后48小时内给予依达拉奉右莰醇可以明显改善90天功能结局,尤其是女性患者获益更大。
参考文献:
Xu J, et al. TASTE Trial Investigators. Edaravone Dexborneol Versus Edaravone Alone for theTreatment of Acute Ischemic Stroke: A Phase III, Randomized, Double-Blind, Comparative Trial. Stroke. 2021 Feb 16:STROKEAHA120031197. doi:
10.1161/STROKEAHA.120.031197.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#AST#
42
#新希望#
69
#卒中患者#
45
许杰何许人也?拥军院长的很多研究的一作都是他
72
参考下
90
真的。
92
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
56