Biological Psychiatr:不同大脑状态的时间占比失衡是 cSVD 相关认知下降的标志
2022-04-16 影像小生 MedSci原创
cSVD的全脑时空共激活模式的特征及其与相关认知缺陷存在相关性
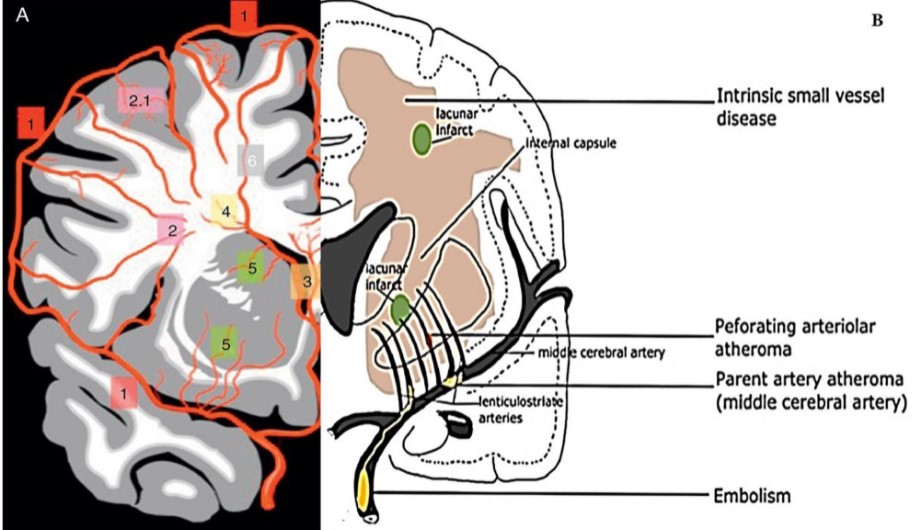
脑小血管病(cSVD)的临床表现包括中风、抑郁和认知障碍。在结构磁共振成像(MRI)上,cSVD可能表现为白质高信号病灶(WMH),在疾病的进程中可能比其他标记物出现更早。认知心理障碍与信息处理和执行功能的缺陷有关。认知障碍是脑小血管疾病 (cSVD) 的标志。功能 MRI 可用于研究分析大脑活动模式与行为变异性之间的联系。
动态功能连接(dFC)研究揭示了无法用静态功能连接方法评估的时空组织,包括多个不同时间分离的同步大脑活动模式的大脑状态。虽然它们的数量仍在争论中,但其科学和临床用途的证据正在积累。对于认知过程的理解进一步受益于dFC方法,因为它检测了不同行为相关的大脑动力学时间尺度和对隐藏在功能连接下的离散事件结构的理解。
汉堡-埃彭多夫大学医学中心Eckhard Schlemm MBBS等在Biological Psychiatry发表题为Equalization of brain state occupancy accompanies cognitive impairment in cerebral small vessel disease研究文章,旨在描述 cSVD 的成像标记、动态连接和认知障碍之间的关联。

该研究通过白质高信号 (WMH) 和骨架化平均扩散率峰宽(PSMD)量化cSVD。静息态 BOLD 信号被聚集成离散的大脑状态,计算了部分占用率 (%) 和停留时间 (s)。使用经过验证的测试评估多个领域的认知。回归分析用于量化白质损伤、空间共激活模式和认知功能之间的关联。
该研究分析了979 名参与者(年龄 45-74 岁,中位 WMH 体积 0.96 ml)的数据

白质病变体积与占用比例(FO) /平均停留时间(DT)之间的关系
- 聚类确定了五种大脑状态,其中在默认模式网络的激活 (+) 或抑制 (-) 状态下花费的时间最多(占用比例:DMN+ 25.1 ± 7.2 %,DMN- 25.5 ± 7.2 %)。
- WMH 体积每增加 4.7 倍,占据 DMN+ 或 DMN- 的几率降低 0.95 倍。
- 在 DMN 相关的大脑状态中花费的时间与执行功能有关。
该研究发现WMH负担的增加与高占比脑状态下的时间减少和低占比脑状态下的时间增加有关。处于默认模式网络状态的时间是执行功能任务中表现不佳的独立预测因子。
该研究首次提出了在cSVD存在的全脑时空共激活模式的特征及其与相关认知缺陷的相关性。缺血性白质疾病的成像标记物与在不同大脑状态的时间的均衡有关,而且,即使以大脑结构损伤为条件,这种去分化也与作为皮层下认知损伤标志的执行功能缺陷有关。
原文出处
Equalization of brain state occupancy accompanies cognitive impairment in cerebral small vessel disease, Biological Psychiatry, 2022, ISSN 0006-3223, https://doi.org/10.1016/j.biopsych.2022.03.019.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#cSVD#
90
#认知下降#
120
#Bio#
76
#Biol#
74