Arch Neurol:顶叶白质高信号预测AD较海马萎缩更敏感
2012-10-02 MedSci MedSci原创
一项新的研究提示,区域性的白质高信号(WMHs)的体积可能比海马萎缩更能预测阿尔茨海默氏(AD)。传统上,海马萎缩被认为是与AD相关的一个影像学标志物,但该研究表明WMHs相较于海马萎缩更能够增加阿尔茨海默病发病风险。这一研究结论发表于最近的《神经病学文献》(Archives Neurology)。 既往研究表明脑内白质高信号,特别是在大脑后半区域的WMH,在那些AD高危风险以及已
一项新的研究提示,区域性的白质高信号(WMHs)的体积可能比海马萎缩更能预测阿尔茨海默氏(AD)。传统上,海马萎缩被认为是与AD相关的一个影像学标志物,但该研究表明WMHs相较于海马萎缩更能够增加阿尔茨海默病发病风险。这一研究结论发表于最近的《神经病学文献》(Archives Neurology)。
既往研究表明脑内白质高信号,特别是在大脑后半区域的WMH,在那些AD高危风险以及已经患有AD患者中是增加的,并可预测AD患者的认知功能下降的速度。一些以人口学为基础的研究表明,WMH的增加与AD的发生相关,但其是否独立于其他的生物标志物,如海马萎缩,还尚不明确。
因此,这项研究入选了717例在2005年和2007年之间接受MRI检查的患者,503例患者完成了为期40个月的随访。而在随访结束时,46例患者被诊断为痴呆(27例为可能AD,6例可能为血管性痴呆,AD例可能为帕金森病痴呆,9例可能是痴呆合并其他疾病)。 结果发现顶叶WMH可预测痴呆发生的时间(风险比HR为1.194,P = 0.03)。根据研究人员计算,顶叶中WMH的体积每增加1立方厘米,其发生痴呆风险增加19%。相对来说,海马体积并不能单独的预测痴呆(HR = 0.419,P = 0.77)。
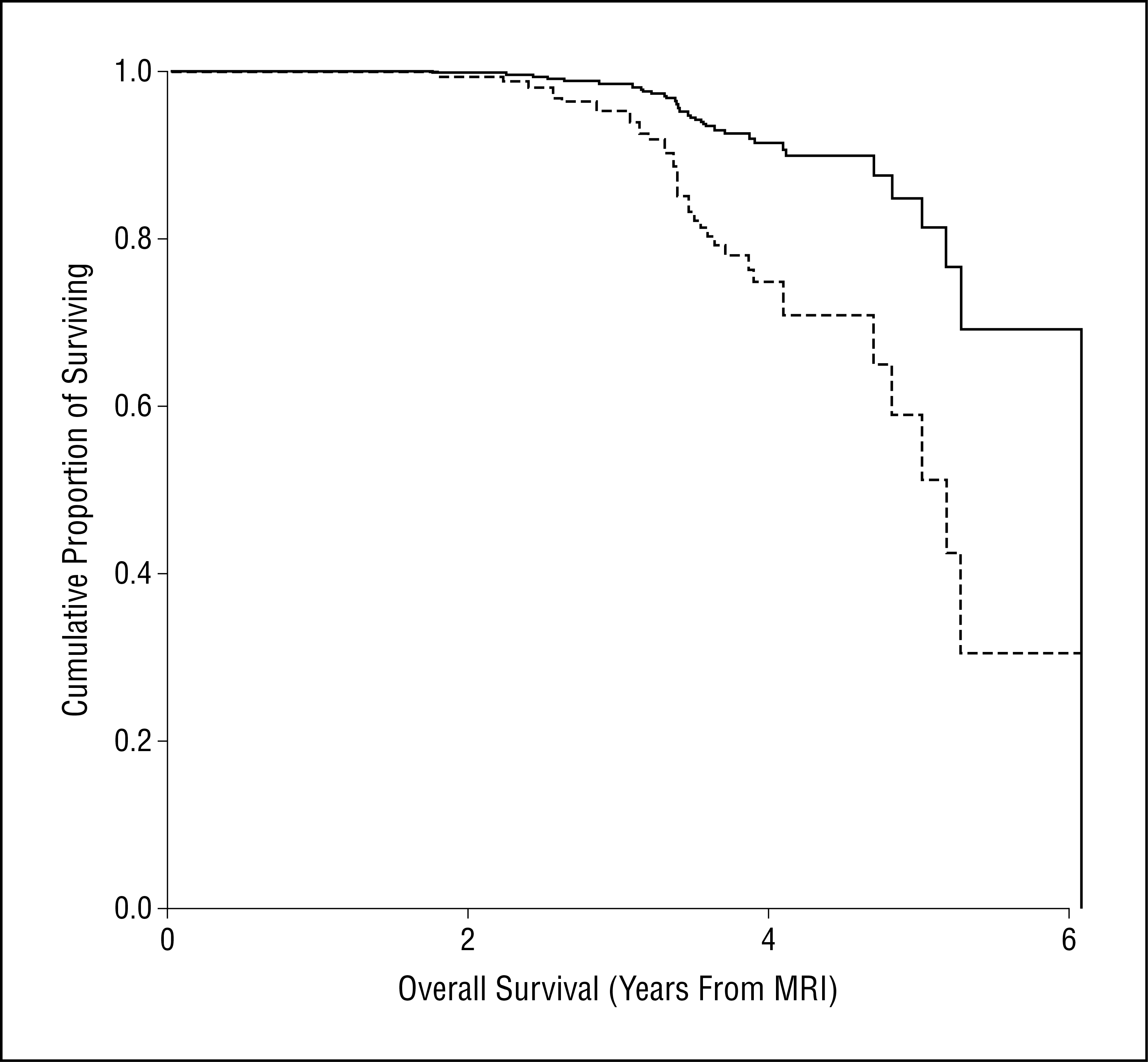
(图示顶叶白质高信号患者[虚线所示]与其他所有患者生存率曲线比较)
尽管之前认为WMH与临床并无太大相关性,但最近其与认知功能的相关性越来越受到关注。研究者称,“我们观察到近期的一些研究均显示WMHs可预测AD和轻度认知功能障碍,同时,WMHs也可预测AD患者认知功能下降的速度。”但这一研究结果仅限于在顶叶,由此引发的问题可能是顶叶在AD的病理变化中发挥重要的作用。
研究者称,“我们的研究表明,通过MRI上的白质高信号(WMHs)可视化的脑小血管病变可能是AD临床表现的征象。”这项研究结果具有临床意义,特别是对于预防阿尔茨海默病。“许多小血管脑血管疾病的危险因素,包括已经明确的高血压,糖尿病,肥胖以及其他的一些危险因素。通过生活方式改变,行为干预,药物治疗,控制这些外周血管因素,可降低脑小血管疾病风险,这反过来可能会减少阿尔茨海默病的风险。"
波特兰俄勒冈AD研究中心的丽莎希尔伯特教授对此研究结果表示认同。她说,顶叶WMHs最能预测阿尔茨海默病这一研究发现是具有创新性的,同时,该研究还强调了检查白质完整性的区域性变化的重要性。另一研究者希尔伯特博士称,“这项研究很有趣,绝对是独一无二的。”
原始文献链接:Regional White Matter Hyperintensity Volume, Not Hippocampal Atrophy, Predicts Incident Alzheimer Disease in the Community
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#萎缩#
85
#白质#
66
#高信号#
64
#Neurol#
65
#白质高信号#
75