JAHA:动脉僵硬度指数和脉压与心血管疾病及死亡的关系!
2018-01-23 xing.T MedSci原创
由此可见,ASI和PP是心血管疾病和死亡结局的独立预测因子。虽然两者都改善了新发疾病的风险预测,但PP似乎比ASI更具有临床价值。
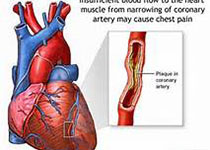
血管老化导致动脉硬化,并可能在心血管疾病(CVD)的发生发展中发挥作用。通过手指容积描记测量的动脉硬化指数(ASI)和脉压(PP)是2个独立的血管老化指标。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员分析了ASI或PP是否能预测社区人群中新发病的心血管病和死亡个体。
研究人员分析了169613名英国生物库的参与者(平均年龄为56.8岁;男性占45.8%),这些患者进行了ASI测量和计算了PP。ASI的平均数±SD为9.30×3.1m/s,PP的平均数±SD为50.98±13.2mmHg。针对CVD中位随访时间为2.8年(四分位距为1.4-4),18190名受试者发生了CVD,其中1587名受试者为心肌梗死(MI)患者,4326名为冠心病患者,1192名为心力衰竭患者和1319名卒中患者。
针对死亡的平均随访长达6.1年(四分位距为5.8-6.3),3678名参与者死亡,其中1180名死于CVD。较高的ASI与总体CVD(校正后的风险比为1.27;95%可信区间[CI]为1.25-1.28)、心肌梗死(1.38;95%CI为1.32-1.44)、冠心病(1.31;95%CI为1.27-1.34)、心衰(1.31;95%CI为1.24-1.37)风险增加相关。ASI还可预测死亡(全因、CVD和其他)。较高的PP与整体CVD(1.57,95% CI为1.55-1.59)、心肌梗死(1.48,95%CI为1.42-1.54)、冠心病(1.47,95%CI为1.43-1.50)、心脏衰竭(1.47,95%CI为1.40-1.55)和CVD死亡(1.47,95%CI为1.40-1.55)风险增加相关。PP可以使非实验室为基础的Framingham风险评分CVD风险重分类改善5.4%,ASI可以改善2.3%。
由此可见,ASI和PP是心血管疾病和死亡结局的独立预测因子。虽然两者都改善了新发疾病的风险预测,但PP似乎比ASI更具有临床价值。
原始出处:
M. Abdullah Said,et al. Relationship of Arterial Stiffness Index and Pulse Pressure With Cardiovascular Disease and Mortality.JAHA.2018. https://doi.org/10.1161/JAHA.117.007621
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






学习了感谢分享
0
#AHA#
57
#血管疾病#
62
#动脉僵硬#
78
#动脉僵硬度#
61
动脉僵硬度指数越高心血管疾病风险越大.
0
谢谢分享.学习了
82
阅
0
学习学习.了解了解
83
学习谢谢分享
66