Obstet Gynecol:未足月诊断子痫前期其死胎风险更大
2015-03-09 Mechront MedSci原创
<span style="font-size:10.5pt;mso-bidi-font-size:11.0pt; font-family:宋体;mso-ascii-font-family:Calibri;mso-ascii-theme-font:minor-latin; mso-fareast-theme-font:minor-fareast;mso-hansi-fon
子痫前期是常见的妊娠相关疾病,以高血压、蛋白尿为主要表现,与死胎风险的增高密切相关。但是目前临床上,对于足月或未足月发生的子痫前期,二者之一谁对母胎危害性更大,尚无定论,因此,Quaker E进行了一项基于人群的队列研究,以探究子痫前期孕周特异性的死胎风险。
该研究纳入了挪威地区1999-2008年554,333名宫内单活胎的孕妇,其中21,020名(3.8%)孕妇为子痫前期,余下533,313名(96.2%)孕妇没有子痫前期。
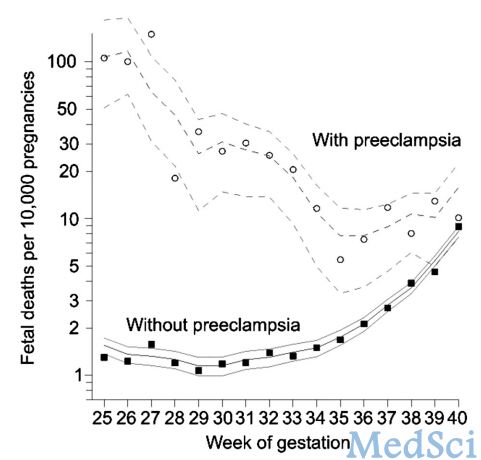
对于研究对象整体而言,每1,000名孕妇中有3.6名是死胎,对于子痫前期群体而言,该数据为5.2/1,000名,其相对危险度RR=1.45,95% CI 1.20-1.76。但是在较早孕周,子痫前期组的死胎数据明显高于不伴子痫前期的孕妇。孕26周,子痫前期组每1,000名孕妇中有11.6名是死胎,而非子痫前期组该数据仅为0.1/1,000,RR=86,95% CI 46-142。研究结果显示,随着子痫前期诊断孕周的增加,其死胎风险呈下降趋势,但是虽然如此,在孕34周,子痫前期组的死胎风险仍高于对照组7倍,该数据不可忽视。
该研究结果表明,死胎风险与子痫前期诊断孕周(即出现子痫前期症状的孕周)密切相关,孕周越小,风险越大。临床上,孕妇一旦诊断子痫前期,需要根据其诊断孕周,评估相应的母胎风险。
原始出处:
Quaker E. Harmon,et al. Risk of Fetal Death With Preeclampsia. Obstet Gynecol 2015;125:628–35
本文系Medsci原创编译整理!转载需要先获得授权,并附原文链接。谢谢!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#TET#
50
#NEC#
62
#子痫前期#
57
#死胎#
77
?
113