Clin Lung Cancer: Atezolizumab联合ipilimumab治疗经治的驱动基因阴性的晚期非小细胞肺癌(NSCLC)的安全性和疗效
2021-09-29 yd2015 MedSci原创
研究表明,Atezolizumab联合ipilimumab治疗经治的驱动基因阴性的晚期非小细胞肺癌显示出一定疗效,并且毒性可控。
目前驱动基因阴性的晚期非小细胞肺癌(NSCLC)的一线标准治疗为免疫治疗单药或联合化疗。免疫检查点抑制剂(ICIs)包括PD1和PD-L1抑制剂。但是PD-L1抑制剂atezolizumab联合CTLA4抑制剂ipilimumab治疗经治的驱动基因阴性的晚期非小细胞肺癌(NSCLC)的疗效不明确。因此,国外研究团队开展了I期临床研究,相关结果发表在Clinical Lung Cancer杂志上。

研究纳入23例患者,既往接受过联合免疫治疗(CPI)的有3例(13.0%)。NSCLC的总体安全人群包括23例患者。Atezolizumab治疗的中位持续时间为4.2个月(0-26个月),中位剂量为5次(1-37次)。大多数患者未错过任何atezolizumab(60.9%)或ipilimumab(95.7%)剂量。
22例(95.7%)患者共报告204例不良事件(AEs)。最常见的AEs为呼吸困难(9例,39.1%)和咳嗽(8例,34.8%)。AEs导致药物剂量改变或中断11例(47.8%);7例(30.4%)患者因毒性停用atezolizumab, 2例(8.7%)患者停用ipilimumab。16例患者出现≥3级AEs(69.6%);其中11例(47.8%)患者认为与治疗相关,最常见的≥3级治疗相关AEs为肺炎(4例,17.4%),淀粉酶升高,脂肪酶升高(4例,17.4%)。13例患者(56.5%)经历了严重的AEs,其中9例患者(39.1%)认为与治疗相关,5例与两种药物相关,2例与atezolizumab和ipilimumab单独相关。报道了2例5级事件,均发生在接受atezolizumab治疗的患者中。5级肺炎被认为与atezolizumab有关,但与ipilimumab无关。
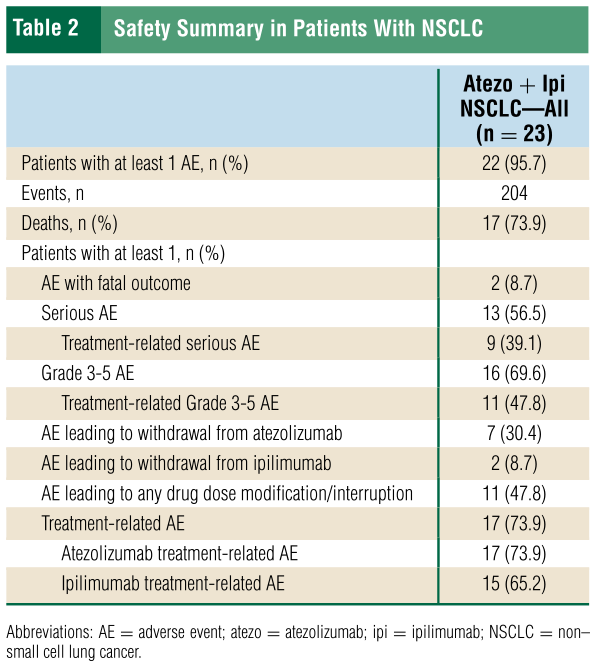
不良事件
总体人群中有6例患者确认为应答,ORR为26.1%。5例应答(25.0%)患者发生在CPI初治NSCLC患者中;3例(15.0%)为CR, 2例(10.0%)为PR。在有反应的患者中位DOR总体为23.0个月(95% CI, 3.2-36.9),在既往未接受过CPI治疗的患者中为36.9个月(95% CI, 2.9-36.9),在接受过CPI治疗的患者中为9.0个月。
既往未接受过CPI治疗NSCLC患者中位生存随访时间为39.7个月(1.2-42.1)。中位PFS为4.2个月(95% CI, 1.7-8.8),中位OS为8.7个月(95% CI, 6.3-15.7)。一年评估的PFS和OS率分别为21.1% (95% CI, 2.7%-39.4%)和38.9% (95%CI,16.4%-61.4%)。

疗效
在接受过CPI治疗的NSCLC患者中位生存随访为39.0个月(3.3-39.0个月);3例患者(100%)均发生PFS事件,2例(66.7%)死亡。中位无进展生存期为2.3个月(95% CI, 1.3-13.1);中位OS为16.2个月(95% CI, 3.3-NE)。一年评估的PFS和OS率分别为33.3% (95% CI, 0.0%-86.7%)和66.7% (95% CI, 13.3%-100%)。
综上,研究表明,Atezolizumab联合ipilimumab治疗经治的驱动基因阴性的晚期非小细胞肺癌显示出一定疗效,并且毒性可控。
原始出处:
Wong DJ, Bauer TM, Gordon MS, et al. Safety and Clinical Activity of Atezolizumab Plus Ipilimumab in Locally Advanced or Metastatic Non-Small Cell Lung Cancer: Results From a Phase 1b Trial. Clin Lung Cancer. 2021 Jul 20:S1525-7304(21)00183-2. doi: 10.1016/j.cllc.2021.07.002. Epub ahead of print. PMID: 34456145.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#非小细胞#
46
#mAb#
47
#驱动基因#
70
#Ipilimumab#
73