这10种疾病容易与“冠心病”混淆,临床上如何鉴别?
2019-03-14 佚名 医学之声
世界卫生组织将冠心病分为5大类:无症状心肌缺血(隐匿性冠心病)、心绞痛、心肌梗死、缺血性心力衰竭(缺血性心脏病)和猝死5种临床类型。我们今天就一起来分享一下,它们应该怎样与那些常见的疾病进行鉴别呢?
世界卫生组织将冠心病分为5大类:无症状心肌缺血(隐匿性冠心病)、心绞痛、心肌梗死、缺血性心力衰竭(缺血性心脏病)和猝死5种临床类型。我们今天就一起来分享一下,它们应该怎样与那些常见的疾病进行鉴别呢?
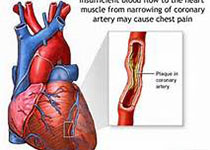
冠状动脉粥样硬化性心脏病是冠状动脉发生粥样硬化病变而引起血管腔狭窄或阻塞,造成心肌缺血、缺氧或坏死而导致的心脏病,常常被称为“冠心病”。但是冠心病的范围可能更广泛,还包括炎症、栓塞等导致的管腔狭窄或闭塞。
一、隐匿型冠心病应与下列疾病鉴别
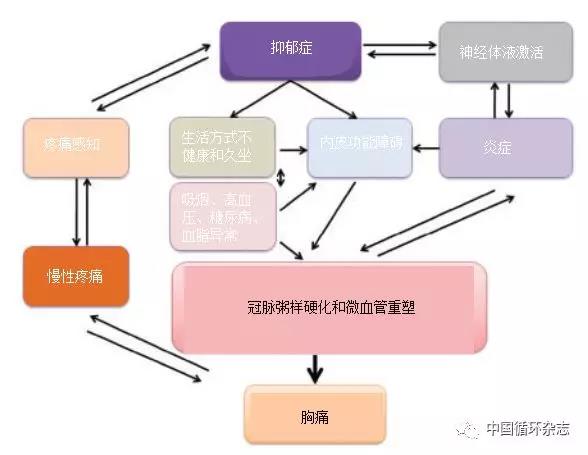
(1)植物神经功能失调:病人多表现为精神紧张和心率增快,在肾上腺素增加的患者,由于心肌氧耗量增加,心电图可有ST段压低或T波倒置。服心得安2小时后心电图多恢复正常。
(2)心肌炎、心肌病、心包病及其他心脏病,电解质失调、内分泌病,药物作用等均可使ST段及T波改变,但据其它临床表现不难排除。
二、心绞痛应与下列疾病鉴别
(1)心脏神经官能症:本病病人常诉胸痛,但为短暂的隐痛,病人常喜叹息,胸痛部位多在左胸乳房下与主尖部位附近,但经常变动,症状多在疲劳之后出现,而不在疲劳的当时、轻度活动反觉舒适,有时可耐受较重的体力活动而不发生胸痛或胸闷。含用硝酸甘油无效或在10多分钟后见效。常伴有心悸、疲乏及其他神经衰弱的症状。
(2)肌肉、骨、关节疾病:如胸肌劳损、颈椎病、胸椎病、肩关节及周围韧带病变、肋软骨炎等,可表现为类似心绞痛症状,但这些病变都有局部压痛,疼痛常与某些姿势及动作有关,局部体检即可明确诊断。
(3)胆管和上消化道病变:如食管裂孔疝、贲门痉挛、胃炎、消化性溃疡、胆石症、胆囊炎等。食管裂孔疝可发生于饱餐后、平卧位,坐起或行走疼痛可缓解。消化性溃疡有与进餐时间相关的规律性,且疼痛时间较长,碱性药物可以缓解。胆石症及胆囊炎疼痛亦为发作性,疼痛时常辗转不安,有局部压痛及黄疽等表现,一般不易误诊。但要注意部分患者同时有胆管疾患和心绞痛,胆绞痛又可引起心绞痛的发作,必须仔细诊断。
三、急性心肌梗死应与下列疾病鉴别
(1)心绞痛:疼痛性质与心梗相似,但发作较频繁,每次发作历时短,一般不超过15分钟,发作前常有诱发因素。不伴有发热、白细胞增加、红细胞沉降率增快或血清心肌酶增高,心电图无变化或有ST段压低或抬高。
(2)急性心包炎:有胸闷胸痛、咳嗽、发热和呼吸困难的病史,但疼痛于深吸气时加重,不伴休克。心电图除aVR导联外,多数导联有ST段呈弓背向下的抬高,无异常Q波。心肌坏死标志物无明显升高。
(3)急性肺动脉栓塞:肺动脉大块栓塞时,常引起胸痛、呼吸困难、休克,但有右心负荷急剧增高的表现。右心室增大,肺动脉瓣区第二心音亢进、三尖瓣区出现收缩期杂音,以及发热及白细胞增加。心电图示电轴右偏,I导联出现S波或原有S波加深,III导联出现Q波和T波倒置,aVR导联出现高R波,胸导联过渡区向左移,右胸导联T波倒置,与心肌梗死的心电图表现不同。
(4)动脉夹层动瘤:亦出现剧烈胸痛,似急性心肌梗塞疼痛性质,但疼痛开始即达高峰,常放射到背、肋、腹、腰及下肢。大部分有明显撕裂样剧痛。双上肢血压及脉搏可有明显差别,少数患者有主动脉关闭不全,可有下肢暂时性瘫痪或偏瘫。CT、超声等可鉴别。
(5)急腹症:急性胰腺炎、消化溃疡穿孔、急性胆囊炎、胆石症等,病人可有上腹部疼痛及休克,可能与本病疼痛波及上腹部者相混,但急腹症多伴消化系统症状,心电图及血清酶测定有助于明确诊断。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










写的不错
71
学习了
82
值得重视
83
学习了很有用不错
81
好
64