Nat Immunol :科学家发现一种新型细胞,可促进中枢神经系统再生!
2020-10-29 探索菌 生物探索
神经退行性疾病是由神经元或其髓鞘的丧失导致人体出现功能障碍的中枢神经系统疾病,包括创伤性脑或脊髓损伤(SCI)、多发性硬化症和运动神经元疾病等。
神经退行性疾病是由神经元或其髓鞘的丧失导致人体出现功能障碍的中枢神经系统疾病,包括创伤性脑或脊髓损伤(SCI)、多发性硬化症和运动神经元疾病等。由于中枢神经系统再生能力差,其损伤康复目前是国际性的医学难题。
当地时间10月26日,《Nature Immunology》发布的一篇文章为治愈这些难治的中枢神经系统疾病提供了新的希望。俄亥俄州立大学和密歇根大学的研究人员发现了一种新型的免疫细胞,不仅可以挽救受损神经细胞免于死亡,还可以再生和修复受损的神经细胞。此外,研究人员还确定了具有类似特征的人类免疫细胞系,可促进神经系统修复。
该报告的第一作者、俄亥俄州立大学神经科学研究所的Andrew Sas博士说:“我们的发现最终可能导致新的免疫疗法的发展,这种疗法可以逆转中枢神经损伤,恢复各种疾病下患者所失去的神经功能。”
促进神经保护和再生的一种潜在策略是调节中枢神经系统损伤的局部免疫反应。当人体出现炎症时,中性粒细胞就会奔赴“战场”,吞噬细胞和细菌。尽管过度活跃的中性粒细胞活动在多发性硬化症、视神经脊髓炎、阿尔茨海默病和中风的情况下会加剧炎症损害,但是越来越多证据表明,这也可能是改善神经系统疾病的突破口。

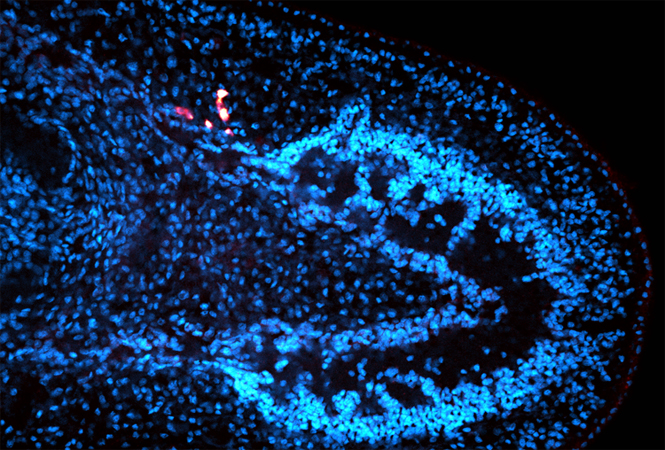
图片来源:俄亥俄州立韦克斯纳医学中心
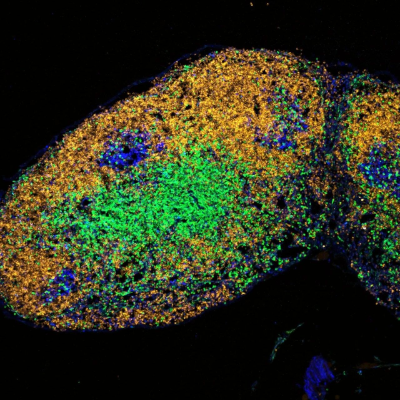
在这项实验中,研究人员发现的是一种新型粒细胞,具有未成熟中性粒细胞的特征,但具有神经保护和神经再生特性。将这种细胞注射给具有视神经损伤或脊髓神经纤维损伤的小鼠体内,能够促进神经元存活和视网膜神经节细胞轴突再生。这种效果部分是通过分泌神经生长因子(NGF)和胰岛素样生长因子(IGF-1)带来的。
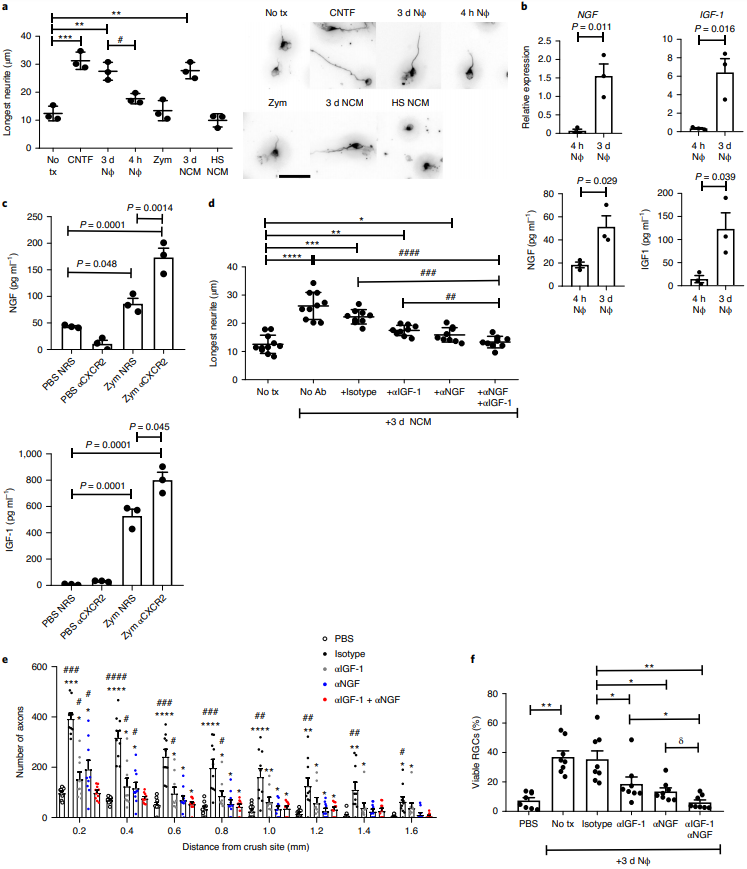
新型细胞部分通过分泌生长因子诱导RGC轴突生长
随后,研究人员测试了具有未成熟中性粒细胞特征的人骨髓细胞在启动神经修复方面的能力。将这类细胞过继转移到RAG1基因缺陷的视神经受损小鼠眼睛后,直接刺激了断裂的视神经节细胞轴突生长。
该报告的通讯作者、俄亥俄州立大学神经科学研究所教授Benjamin Segal说:“这种免疫细胞亚群分泌的生长因子可增强中枢神经系统创伤后神经细胞的存活,刺激断裂的神经纤维在中枢神经系统中再生,这确实史无前例。”
接下来,研究人员将继续对这种细胞进行探索并在实验室中将其扩增,从而增强治疗效果。他们希望,未来这些细胞能够帮助患者减缓或停止进行性神经功能衰退。
原始出处:
Andrew R Sas, Kevin S Carbaja, Andrew D Jerome,et al. A new neutrophil subset promotes CNS neuron survival and axon regeneration.Nat Immunol. 2020 Oct 26. doi: 10.1038/s41590-020-00813-0.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#科学家发现#
46
#Nat#
44
#神经系统#
28
#中枢神经#
38