Lancet Oncol.:恩杂鲁胺测改善转移性去势抵抗前列腺癌患者生活质量(PREVAIL试验)
2015-05-08 Jessie 译 MedSci原创
Normal 0 10 pt 0 2 false false false EN-US ZH-CN X-NONE
 恩杂鲁胺可显著改善转移性去势抵抗前列腺癌患者的健康相关生活质量、疼痛,并延迟初次化疗患者的首发骨髓相关事件的发生。近期发表在Lancet Oncol.上的一篇文章报道了III期PREVAIL试验中关于患者健康相关生活质量、疼痛及骨髓相关事件的研究结果。
恩杂鲁胺可显著改善转移性去势抵抗前列腺癌患者的健康相关生活质量、疼痛,并延迟初次化疗患者的首发骨髓相关事件的发生。近期发表在Lancet Oncol.上的一篇文章报道了III期PREVAIL试验中关于患者健康相关生活质量、疼痛及骨髓相关事件的研究结果。
之前报道了PREVAIL试验发现,恩杂鲁胺可显著提高无症状、轻微症状及初次化疗的转移性去势抵抗这三组前列腺癌患者的总生存时间和影像学无进展生存时间。这篇文章里,研究者报道了PREVAIL试验中恩杂鲁胺对健康相关生活质量、疼痛及骨髓相关事件的作用。
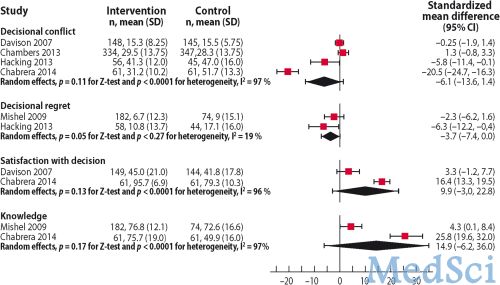
试验中进行了双盲,患者随机分入恩杂鲁胺组(n=872)和安慰剂组(n=845),剂量均为160mg/天。健康相关生活质量的评估使用前列腺癌患者生活治疗问卷(FACT-P)和EQ-5D问卷,评估时间为基线时、治疗期间。疼痛的评估使用简版简明疼痛清单(BPI-SF),评估时间分别为招募时、基线、治疗13周及25周。生活质量的分析应用混合效应模型检测基线至61周的生活质量得分的最小平方均分的变化。收集了骨髓相关事件的发生比例和首发时间。
干预组和安慰剂组的中位治疗时长分别为16.6个月和4.6个月。混合效应模型显示,干预组与安慰机组相比,生活质量FACT-P的基线与61周得分变化存在显著差异,EQ-5D视觉模拟评分的结果也存在显著差异。干预组生活质量开始下降的时间点为11.3(95%CI:11.1~13.9)个月,对照组为5.6(95%CI:5.5~5.6)个月,危险比(HR)为0.62(95%CI:0.54~0.72,P<0.0001)。干预组生活质量(FACT-P)显著提高的患者比例为40%(327/826),对照组为23%(181/790);EQ-5D效用指数评估的结果为28% vs. 16%,视觉模拟评分的结果为27% vs. 18%,均具有统计学意义(P<0.0001)。
干预组和安慰机组BPI-SF评估的疼痛进展到最严重的时间分别是5.7(5.6~5.7)个月和5.6(5.4~5.6)个月(HR=0.62,95%CI:0.53~0.74;P<0.0001)。13周时,干预组疼痛达到最严重的比例显著低于安慰机组(29% vs. 42%,P<0.0001),但25周时结果没有显著差异(32% vs. 38%,P=0.068)。
到数据截点时,干预组32%的患者出现了骨髓相关事件,安慰机组的这一比例为37%。首发骨髓相关事件的中位时间在干预组为31.1个月,安慰机组为31.3个月(HR=0.72,95%CI:0.61~0.84;P<0.0001)。
可见,恩杂鲁胺不仅能够延长转移性去势抵抗前列腺癌患者的生存时间,而且能提高患者的生活质量,改善疼痛及骨髓相关事件的发生。
原始出处
Loriot Y, Miller K, Sternberg CN, Fizazi K, De Bono JS, Chowdhury S, Higano CS, Noonberg S, Holmstrom S, Mansbach H, Perabo FG, Phung D, Ivanescu C, Skaltsa K, Beer TM, Tombal B. Effect of enzalutamide on health-related quality of life, pain, and skeletal-related events in asymptomatic and minimally symptomatic, chemotherapy-naive patients with metastatic castration-resistant prostate cancer (PREVAIL): results from a randomised, phase 3 trial.Lancet Oncol. 2015 May;16(5):509-21. doi: 10.1016/S1470-2045(15)70113-0. Epub 2015 Apr 14.
本文是MedSci编译,欢迎转载,转载请注明出处,非常感谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Lancet#
77
#去势抵抗前列腺癌#
84
#Oncol#
68
看看
159
#转移性#
117