OCC 2016:钱菊英——血管痉挛性心绞痛诊治及中国专家共识解读
2016-05-26 MedSci MedSci原创
第十届东方心脏病学会议(The 10th Oriental Congress of Cardiology,OCC 2016)于今天开始在上海世博中心(浦东新区世博大道 1500 号) 召开。梅斯医学(MedSci)作为官方媒体受邀参加此次大会。 在今天早上的2016年上海市医学会心血管病分会年会上,第十届东方心脏病学会议大会秘书长、复旦大学附属中山医院心内
第十届东方心脏病学会议(The 10th Oriental Congress of Cardiology,OCC 2016)于今天开始在上海世博中心(浦东新区世博大道 1500 号) 召开。梅斯医学(MedSci)作为官方媒体受邀参加此次大会。
在今天早上的2016年上海市医学会心血管病分会年会上,第十届东方心脏病学会议大会秘书长、复旦大学附属中山医院心内科副主任医师、钱菊英教授做了题为《血管痉挛性心绞痛诊治及中国专家共识解读》的精彩演讲。
一、为什么制定中国共识?
1、发病率高
日本多中心研究显示,冠脉粥样硬化的胸痛患者中,乙酰胆碱试验阳性率43%。
2014年Circulation发表的临床基本特征相似的921例高加索人的阳性率为33.4%
2、并非良性疾病:
大部分患者对药物治疗(CCB、Nirtrates)效果良好,但5%~30%为药物难治性。
大部分患者预后良好,大部分可诱导AMI和恶性心律失常,心源性猝死率2%~16%。
3、了解不足
80年代前痉挛机制曾一度被认为是心绞痛的主要机制
80年代后血栓机制深入人心,而痉挛备受忽视
二、血管痉挛性心绞痛的概念演变
1、变异性心绞痛:静息性胸痛发作时检测到一过性ST段抬高
2、血管痉挛性心绞痛:ST段压低性心绞痛更多见;运动也可诱发;现在常用这个概念
3、冠状动脉痉挛综合征:冠脉痉挛广泛参与心脏病发生发展(不常用)
三、危险因素
1、主要危险因素:吸烟和血脂代谢紊乱(分别使CASS风险增加3.2倍和1.3倍)
2、其他诱因:可卡因、酗酒、介入、过敏、扩冠药物停用
3、非危险因素:如高血压、糖尿病

好发于40岁以上的人群,男性比女性多见
四、发病机制
1、血管内皮结构和功能紊乱:ET/NO比值升高
2、血管平滑肌反应性增高:Rho激酶途径
3、自主神经功能障碍:发作时迷走活性占优
4、遗传易感性:与NO合酶相关基因等
五、典型CAS性心绞痛(变异型心绞痛)的特点
1、有吸烟、血脂异常、可卡因、酗酒、高血压、糖尿病等危险因素
2、发作有昼夜节律(后半夜)至上午发作多见
3、运动耐量昼夜变化:清晨轻微劳力即可诱发,午后剧烈活动也不会诱发
4、典型者的心电图有一过性ST段抬高和T波高耸
5、冠状动脉造影多可见动脉硬化斑块;激发试验多诱发出局限性或节段性痉挛。
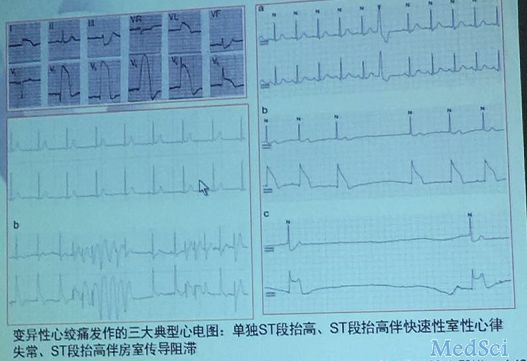
变异性心绞痛发作三大典型心电图:单独ST段抬高、ST段抬高伴快速性室性心律失常、ST段抬高伴房室传导阻滞。
六、冠脉痉挛的临床表现及诊断
冠脉痉挛的临床表现常具有复杂性
1、ST段下移更为常见冠脉痉挛时心电图ST段下移和(或)T波倒置较ST段抬高更为常见,病理基础为冠脉闭塞不完全或伴侧支形成,产生非透壁性心肌缺血。即非典型CAS性心绞痛。
2、无症状性缺血更为常见
CAS所引起的无症状性心肌缺血较常见,动态心电图监测可表现为ST段抬高或压低,而无明显症状。
3、可能以猝死或晕厥为首发症状
左冠状动脉痉挛多表现为室性心律失常,严重者可发生室性心动过速、室颤、甚至猝死。
右冠状动脉痉挛则多表现为心动过缓、窦性停搏或完全性房室传导阻滞。
若猝死前有大量吸烟、吸毒或大量饮酒病史,更应高度怀疑CAS诱发严重心律失常所致。
4、冠脉痉挛性AMI
闭塞性痉挛持续不能缓解即AMI;常有精神创伤、过度劳累、大量烟酒、吸毒史。
症状缓解或在冠脉硝甘后,造影显示无显著狭窄;长时痉挛可继发血栓,但抽烟后多无显著残余狭窄。
5、CAS诱发心力衰竭
严重的一过性缺血可导致暂时性室壁运动异常,诱发一过性心衰。冠脉痉挛反复发作可使心肌冬眠,降低心肌收缩力,诱发慢性左室功能障碍,抗痉挛治疗对这些心衰患者有效。
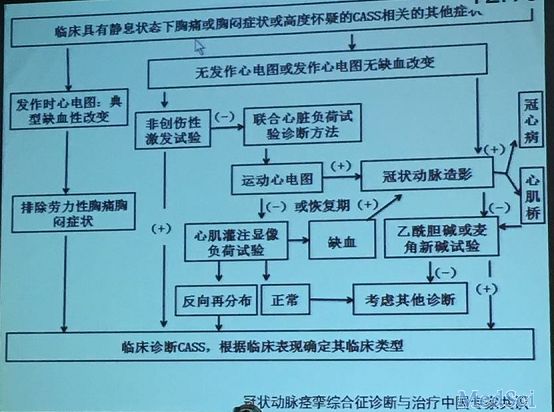
冠状动脉痉挛综合征诊断与治疗中国专家共识
冠脉痉挛诊断时,常规检查价值有限
1、心电图:虽然静息性胸痛合并一过性ST段抬高可直接临床诊断,但只有极少数患者能及时行心电图检查。而且,ST段压低更为多见,无法确诊。
2、动态心电图:并不一定能捕捉到CAS发作(上午检查的效果会较好)
3、运动平板试验:白天甚少发作,价值有限
4、冠脉造影:发现自发痉挛的概率极低
5、激发试验:
非创伤性激发试验因敏感性太低难以满足诊断要求。
创伤性药物激发试验(麦角新碱、乙酰胆碱):是目前诊断CASS的“金标准”,但存在安全隐患。
七、治疗
1、急性发作期治疗
急性发作时,舌下含服TG常可缓解胸痛
如不缓解,可静脉或冠脉使用硝酸酯类
如不缓解,加用口服或静脉短效快效CCB
冠脉痉挛急诊处理原则:
冠脉痉挛性室颤和心跳骤停:除颤基础上硝酸酯类扩冠治疗
冠脉痉挛性心源性休克:IABP基础上硝酸酯类扩冠治疗;肾上腺素和多巴胺可能加重痉挛
冠脉痉挛性心律失常:抗心律失常药作用甚微
明确室颤和心跳骤停是否与冠脉痉挛有关非常重要
临床上遇见伴有显著ST段改变、难治性室速室颤、三度AVB时,应考虑到冠脉痉挛的可能
2、稳定期治疗
(1)控制诱发因素:戒烟、戒酒、控制血压、维持适当的体重、纠正糖、脂代谢紊乱、避免过度劳累、勿随意停用扩冠药物等
(2)扩冠治疗
一线:CCB,抑制血管平滑肌Ca2+内流,解除痉挛,首选用药(几乎没有禁忌症)
二线:硝酸酯类,松弛血管平滑肌(存在耐药现象)
三线:选择性α阻滞剂哌唑嗪、KATP开放剂尼克地尔、Rho激酶抑制剂法舒地尔、静脉镁
(3)其他药物:他汀类、抗血小板药、β受体阻滞剂(对无冠脉狭窄的CASS患者禁忌单独使用)
(4)给药时间:晚上睡前服用
3、ICD治疗
共识指出:对于因CAS诱发的持续性实行心动过速或室颤等所导致的心脏骤停存活患者中,在规范药物治疗下仍反复发作者,可在进行充分评估的基础上考虑安装埋藏式自动除颤起搏器。
4、支架治疗
共识指出:CASS患者原则上不主张介入治疗,个案报告显示,中重度冠状动脉狭窄基础上合并CAS可能从介入治疗中获益。
八、小结
1、VSA并不少见,常以“疑难病例”形象出现
2、并非良性疾病,治疗不当可猝死
3、戒烟是前提,CCB是基础
4、高危者可器械治疗,但证据不足

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










我想问一下,抗血小板是选用单抗还是双抗?
91
#专家共识#
70
#血管痉挛#
148
#中国专家共识#
94
#钱菊英#
80
#痉挛#
78
#OCC#
76
第一次看到,很有意思
164
第一次看到,很有意思
173