Int J Radiat Oncol Biol Phys:晚期胰腺癌适不适合放化疗,中性粒细胞计数有提示!
2021-04-02 Nebula MedSci原创
中性粒细胞计数的变化可预测晚期胰腺癌患者从放化疗中的获益高低!
胰腺癌是全球癌症相关死亡的主要原因之一,五年存活率不超过10%。约80%的患者在确诊时已是局部晚期或存在远处转移。诱导化疗或有助于筛选预后较好的患者,但局部晚期胰腺癌(LAPC)诱导化疗后的管理策略仍存在争议,特别是放化疗的作用。
在这种情况下,能够预测总存活率(OS)、鉴定需要强化诱导方案和从放化疗中获益的患者的生物标志物显得尤为必要。
近日发表在Int J Radiat Oncol Biol Phys上的“Predictive Value of Neutrophils Count for Local Tumor Control After Chemoradiotherapy in Patients With Locally Advanced Pancreatic Carcinoma”研究探究了基线中性粒细胞计数是否可预测LAPC患者的OS。
国际性多中心的随机3期试验(LAP07)纳入了442例LAPC患者。Antoine等研究人员分析了基线中性粒细胞(中性粒细胞计数>7g/L)和中性粒细胞计数升高(中性粒细胞增多症)或诱导化疗后中性粒细胞绝对计数较基线增加对OS、无进展生存期和局部控制(LC)的预测价值。
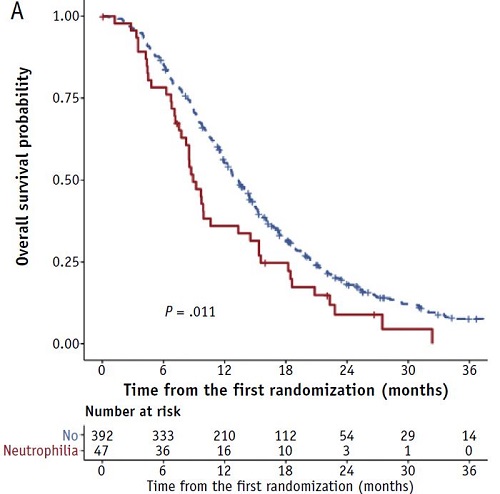
基线有无中性粒细胞增多症的患者的预后
在442例患者中,47例(11%)中性粒细胞增多症患者的OS较差(中位数 8.9个月 vs 13.3个月;P=0.01)。诱导化疗后,在235例血细胞计数正常的患者中,90例(38%)患者的中性粒细胞计数升高,在单因素和多因素分析中,诱导化疗后中性粒细胞计数升高都与患者的OS降低相关(单因素分析中位数:14.4个月 vs 17.9个月;P=0.001;多因素分析P=0.004)。
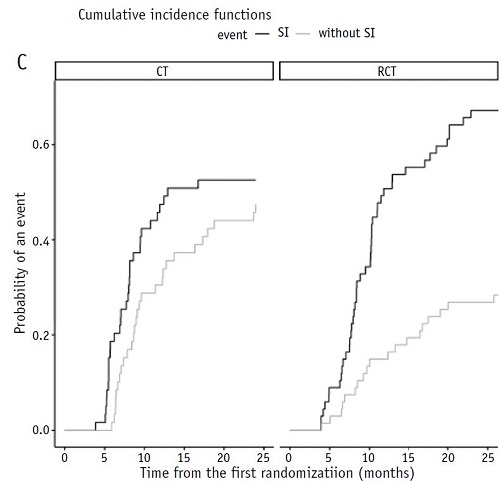
有无系统炎症(SI)的患者采用CT或RCT治疗的累积复发率
此外,中性粒细胞计数升高还预示放化疗对局部控制的疗效收益降低。在126例中性粒细胞计数没有升高的患者中,放化疗组的1年局部控制率为80%,化疗组的为54%(P<0.001;交互测试P=0.015)。
综上,该研究表明,在LAPC患者中,基线中性粒细胞增多症和中性粒细胞计数绝对增加与OS更差相关。此外,中性粒细胞计数是一个独立的预后因素,也是一个强有力的局部控制率的预测生物标志物,对放化疗的益处具有很强的预测性。中性粒细胞计数的评估有助于筛选诱导化疗后可能受益于放化疗的患者。
原始出处:
Schernberg Antoine,Vernerey Dewi,Goldstein David et al. Predictive Value of Neutrophils Count for Local Tumor Control After Chemoradiotherapy in Patients With Locally Advanced Pancreatic Carcinoma. Int J Radiat Oncol Biol Phys, 2021, https://doi.org/10.1016/j.ijrobp.2021.01.052
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#DIA#
82
#Oncol#
96
#Bio#
85
#Biol#
80
#放化疗#
85
#中性粒细胞#
73
#晚期胰腺癌#
96
胰腺癌是全球癌症相关死亡的主要原因之一。
105
LNR
109
谢谢梅斯分享这么多精彩信息
81