二维超声联合剪切波技术诊断新生儿假两性畸形1例
2019-02-11 张旭 田瑞 段菲 医学影像学杂志
二维超声声像图联合声触诊组织量化(VTQ)技术对两性畸形的诊断是一项新技术,报道极少,现报道应用于典型的男性假两性畸形1例如下。
二维超声声像图联合声触诊组织量化(VTQ)技术对两性畸形的诊断是一项新技术,报道极少,现报道应用于典型的男性假两性畸形1例如下。
本例患儿社会性别女性,40天,足月顺产,出生时大阴唇饱满,未予重视,监护人诉患儿近期频繁哭闹,食欲欠佳,排尿部位异常,尿液似由“阴蒂”排出,遂来我院就诊。
查体:患儿身高54.0 cm,体重5.3kg。阴蒂肥大,两侧阴唇饱满。四肢无畸形,肌力及肌张力正常。父母非近亲结婚,无家族性遗传病史。超声所见:盆腔内未探及明显子宫附件回声,膀胱颈处似可见前列腺回声,大小约1.5 cm×1.4 cm×1.0 cm(图1),回声尚均。双侧大阴唇深面均可见睾丸附睾回声,右侧大小66mm×12mm×25mm,左侧大小为73mm×12mm×19mm,测量睾丸剪切波的平均值为0.73m/s(图2)。双侧睾丸周围可见无回声区环绕,左侧深约0.53 cm,右侧深约0.75 cm(图3)。
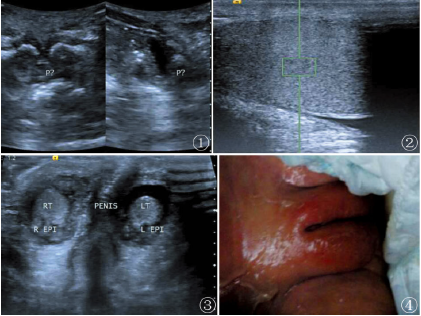
图1膀胱颈处探及前列腺回声;图2睾丸的剪切波值测量;图3双侧睾丸及阴茎回声;图4患儿女性外阴表现
于耻骨联合下方皮肤内可见部分阴茎回声,呈屈曲状,长约1.0 cm。超声提示:1)符合假两性畸形超声表现,建议结合相关检查;2)双侧睾丸鞘膜积液3)子宫附件未探及。染色体检查为染色体核型46XY。
讨论:
两性畸形是一种性别畸形,发病率约1/10万至1/30万,大多数患者确诊一般在出生时。临床表现复杂多样,可分真两性畸形和假两性畸形,假两性畸形又可分为男性假两性畸形与女性假两性畸形真两性畸形是在机体内同时存在两种性别的生殖器官,睾丸和卵巢等性腺。核型可为正常男性型、女性型或嵌合型,外生殖器和生殖导管表现为两性畸形。男性假两性畸形是指核型为46XY,性腺为睾丸,有相对正常或发育不全的男性内生殖器官,外生殖器及第二性征发育出现不同程度女性化,可伴发育程度不等的女性内、外生殖器。
本例患儿出生后40天,因排尿部位异常就诊,生殖器表现虽然为女性,但是盆腔内未发现子宫及卵巢,在大阴唇深面可见发育不完全的睾丸,与既往文献报道一致。有研究表明可能与同家族遗传有关,X连锁隐性遗传或限男性的常染色体显性遗传;追问病史,患儿父母无家族病史,考虑可能是由于胚胎时期的性腺分化异常导致;结合超声表现、染色体分型(46XY型)考虑男性假两性畸形。本例患者为男性假两性畸形,手术方式的选择需要结合后续内外生殖器的发育情况、患者及家属的意愿以及手术后的社会适应能力两性畸形的治疗不仅仅是外科手术治疗,还包括内分泌治疗以及心理治疗多学科综合治疗。
超声对两性畸形的诊断、治疗及预后有着非常重要意义。首先,超声可以实时的观察人体内部脏器,对确定生殖器官的有无,了解其存在的部位,测量其大小,观察其形态,为性别畸形的诊断提供解剖学上的依据。其次,超声作为一种无创的检查手段,对于生殖器官的显像敏感性非常高,非常适合患者多次重复检查及术后复查。再次,联合声触诊组织量化技术(VTQ),通过探头发射脉冲声波使组织产生形变,定量测量组织的硬度,得到相应的数值,判断所测组织的性质,克服了单纯使用二维超声的主观性,是一种较为客观且简单易操作的影像学方法。既往研究证实在肝脏、甲状腺、乳腺肿瘤的临床研究中,VTQ技术准确性较高,与病理组织相关性基本一致。
此病例测量的剪切波的平均值符合正常男性睾丸的正常范围,与既往研究基本一致。二维超声联合VTQ技术能进一步提高疾病的诊断准确率。综上所述,超声作为一种实时、无创、可重复性强的影像学检查手段,对两性畸形的发现、治疗、预后等有着非常重大的意义。
原始出处:
张旭,田瑞,段菲,栗建辉.二维超声联合剪切波技术诊断新生儿假两性畸形1例[J].医学影像学杂志,2018(01):170-171.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#两性#
77
#剪切波#
66
#二维超声#
62
#畸形#
67