Circulation:调控动脉粥样硬化中的炎症和纤维增生性的新机制
2017-05-16 MedSci MedSci原创
动脉粥样硬化斑块形成是由血管壁的慢性炎症和纤维增生性重塑引起的。以前有研究证实,人和小鼠的动脉粥样硬化斑块都显示出EphA2的表达升高。EphA2是参与细胞-细胞相互作用和肿瘤发生的指导分子。近期,一项发表在杂志KIdney Int上的研究通过在动脉粥样硬化(Apoe-/-)的小鼠模型中敲除EphA2并通过评估多种血管细胞培养模型中的EphA2功能来评估EphA2在动脉粥样硬化中的作用。喂养8-1
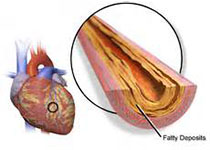
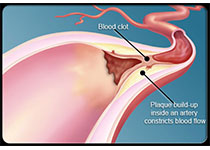
动脉粥样硬化斑块形成是由血管壁的慢性炎症和纤维增生性重塑引起的。以前有研究证实,人和小鼠的动脉粥样硬化斑块都显示出EphA2的表达升高。EphA2是参与细胞-细胞相互作用和肿瘤发生的指导分子。
近期,一项发表在杂志Circulation上的研究通过在动脉粥样硬化(Apoe-/-)的小鼠模型中敲除EphA2并通过评估多种血管细胞培养模型中的EphA2功能来评估EphA2在动脉粥样硬化中的作用。喂养8-16周后,研究者们评估了西方饮食、雄性和雌性小鼠在大血管中的动脉粥样硬化负荷,并分析了血浆脂质水平。
相比之下,内皮EphA2敲低显着降低流动下的单核细胞粘连。此外,EphA2-/-Apoe-/-小鼠显示出来进展到晚期动脉粥样硬化斑块的减少以及平滑肌和胶原含量减少。与这种表型一致的是,EphA2在平滑肌转化为合成表型后显示出增强的表达,并且EphA2消耗减少动脉粥样硬化斑块和培养的血管平滑肌细胞中的平滑肌增殖,促有丝分裂信号和细胞外基质沉积。
此项研究表明:EphA2在动脉粥样硬化中具有新的作用,可以调节斑块炎症和进展为晚期动脉粥样硬化病变。细胞培养研究表明内皮EphA2通过促进单核细胞粘附而促进动脉粥样硬化性炎症,而平滑肌EphA2表达可通过调节平滑肌增殖和细胞外基质沉积来调节进展为晚期的动脉粥样硬化。
原始出处:
Finney AC, Funk SD, et al. EphA2 Expression Regulates Inflammation and Fibroproliferative Remodeling in Atherosclerosis. Circulation. 2017 May 9. pii: CIRCULATIONAHA.116.026644. doi: 10.1161/CIRCULATIONAHA.116.026644.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粥样硬化#
68
#增生性#
66
学习了,。。。。。
92
学习了
78