International Journal of Cancer:表观遗传新应用!宫颈癌检测率 100%!
2018-12-19 佚名 转化医学网
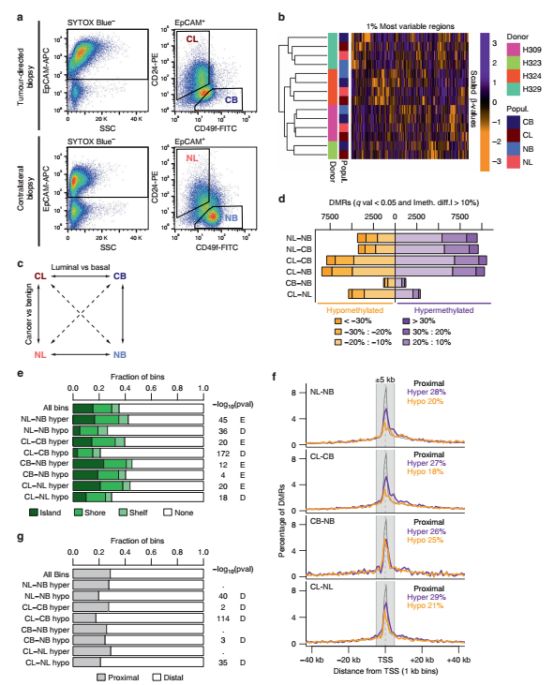
导 读 宫颈癌是一种最常见的女性生殖道恶性肿瘤,发病率在女性恶性肿瘤中居第二位,多发于发展中国家,每年有超过 26 万的妇女死于宫颈癌。在推崇精准医疗的当下,宫颈癌的提早检测提早预防是许多研究者的课题,伦敦 Queen Mary 大学的研究者们,在分析了 15744 份女性的临床筛查数据后发现,可以使用一种新的成本较低的基于表观遗传学的检测方法,较为有效的在早期检测宫颈癌。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#eRNA#
66
#Nat#
56
#宫颈#
56
学习
104
已学习
84