累及鼻中隔的Rosai-Dorfman病2例
2018-05-17 沈暘 洪苏玲 柯霞 临床耳鼻咽喉头颈外科杂志
患者,女,41岁,因“发现鼻背肿物4个月,加重伴鼻塞2个月”就诊于我院。
例1
【一般资料】
患者,女,41岁,
【主诉】
因“发现鼻背肿物4个月,加重伴鼻塞2个月”就诊于我院。
【现病史】
入院前4个月,患者无明显诱因出现鼻背部红色肿物,约黄豆大小,曾在当地医院皮肤科就诊,外用药物(具体不详)治疗后症状无缓解。入院前2个月,患者鼻背肿物逐渐增大,伴外鼻肿胀。当地医院鼻窦CT检查示:鼻梁肿胀,鼻部皮下至鼻中隔结节。行鼻腔新生物活检示:纤维组织增生,伴大量淋巴细胞浸润,泡沫样巨噬细胞增生,形成非典型肉芽肿样病变,特殊染色显示巨噬细胞胞质内外有颗粒状微生物。患者至我院就诊,门诊以“鼻腔新生物”收入我科。
【体格检查】
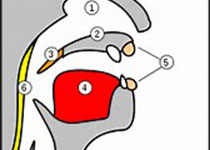
患者一般情况良好,全身浅表淋巴结未扪及肿大。专科体检见外鼻肿胀明显,鼻背可见红色肿物隆起,双侧鼻腔黏膜肿胀明显,鼻中隔前份膨隆,左侧淡红色、质地较韧新生物,边界不清,表面光滑,双侧中鼻道狭窄。
【辅助检查】
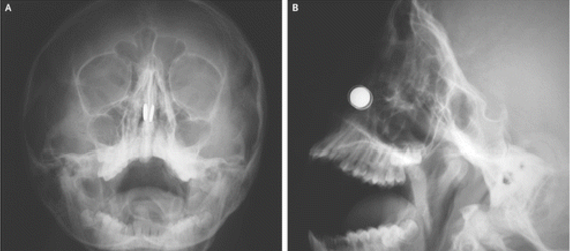
入院后于行鼻窦CT示:鼻根部及鼻中隔区见结节状软组织密度影,大小约25mm×21mm,密度均匀,增强后强化较均匀,相邻鼻骨骨质吸收变薄,双侧上颌窦少许炎症。入院后2d行鼻中隔新生物活检示:大量淋巴细胞、浆细胞及吞噬活跃的组织细胞浸润;免疫组织化学检测示:CD68(+),溶菌酶(+),S100(+),Ki678%(+),CD1α(-),
【初步诊断】
符合窦组织细胞增生伴巨大淋巴结病(Rosai-Dorfman病)。
【治疗】
在全身麻醉下行鼻内镜下鼻腔病损切除术,术中见鼻中隔前份明显膨隆,左侧暗红色新生物,边界不清,质稍韧,骨质吸收。完整切除病变组织,保留完整鼻中隔右侧黏膜。术后病理检查示:符合Rosai-Dorfman病。术后半年随访,鼻内镜检查见双侧鼻腔通气良好,未见复发征象。
例2
【一般资料】
患者,女,25岁,
【主诉】
因“反复双侧鼻塞4个月”就诊于我院。
【现病史】
入院前4个月,患者无明显诱因出现双侧鼻塞,左侧尤甚,晨起加重,偶伴脓涕,未予重视。入院前2周患者自觉症状稍加重,至当地医院就诊。纤维喉镜示:鼻腔新生物,鼻中隔偏曲。MRI检查示:双侧鼻道增多异常软组织信号影,肉芽肿?并全组鼻窦炎,鼻中隔左偏,双侧腮腺组、咽喉组及颈部Ⅱ区多发淋巴结显示,部分肿大。行鼻腔新生物活检示:左右鼻腔符合Rosai-Dorfman病。为求进一步诊治,患者入我科住院治疗。
【体格检查】
患者一般情况良好,颈部Ⅱ区扪及多个肿大淋巴结,质韧、边界清、活动度可,最大直径约2cm。专科体检见鼻外观无畸形,双侧鼻腔肿胀、狭窄,鼻中隔左偏,总鼻道脓性分泌物。
【辅助检查】
【治疗】
入院后第3天在全身麻醉下行鼻腔肿瘤切除加鼻中隔成形术;术中见鼻中隔左偏,中份膨隆,黏膜粗糙,骨质缺损,双侧中鼻道及下鼻甲表面见暗红色新生物,质稍韧,边界不清,触之易出血。完整切除病变组织并行鼻中隔成形术。术后病理检查示:符合Rosai-Dorfman病。术后半年随访,未见复发征象。
【讨论】
Rosai-Dorfman病又称为窦组织细胞增生症伴巨淋巴结病,是起源于骨髓干细胞的非肿瘤性良性组织细胞增生性疾病。1969年Rosai与Dorfman首次对本病进行了详细报道,故又称之为RD病(Rosai-Dorfman disease,RDD)。好发于儿童和青少年,男女发病比例约2:1。其病因尚不明确,可能与病毒感染和免疫功能障碍有关。鼻腔鼻窦的RDD临床表现多样,缺乏特征性表现,易误诊。RDD是起源于骨髓干细胞的非肿瘤性良性组织细胞增生性疾病。根据病变累及范围,RDD可分3种亚型:淋巴结型、结外型和混合型(同时累及淋巴结和结外器官)。从数十年国内外文献报道来看,RDD最常见的为淋巴结型,主要表现为颈部淋巴结多发无痛性中等硬度的肿大;混合型占约40%,结外受累部位多见于,有皮肤、鼻腔鼻窦、眼眶、骨、腮腺等,少数病例累及内脏器官如肺、肾、肝则提示预后不良;约5%单独发生于淋巴结外,不伴淋巴结肿大及相应的系统性功能异常(结外型)。发生于鼻腔鼻窦的结外RDD多无特征性临床表现和影像学改变,因此该病常常很难得到早期准确诊断,易误诊。本文中第1例患者仅表现为起源于鼻中隔黏膜的鼻腔新生物,未发现伴肿大淋巴结证据,故考虑为结外型;第2例患者除鼻腔新生物,体检及影像学检查均提示腮腺组、咽喉组及颈部Ⅱ区多发淋巴结肿大,考虑为混合型。因我们起初对该疾病的认识有限,未行相关检查了解患者肺、肾、肝等是否有累及,故对病情的评估尚局限。RDD的确诊依赖于组织病理学检查,主要表现为大量成熟的浆细胞和淋巴细胞浸润,不同形态的组织细胞增生,增生的细胞分化良好,体积大,细胞形态一致,胞质丰富淡染嗜酸性或较透明,有时胞质呈泡沫状,并可见梭形的组织细胞,细胞核呈大的空泡状,染色质呈细颗粒状,分布均匀,核分裂很少见。本病特征性的病理改变是组织细胞的胞质中可见吞噬的淋巴细胞,免疫组织化学检测结果显示组织细胞呈S100(+)、CD68(+)阳性和CD1(-)。相对于淋巴结内RRD而言,原发于鼻腔及鼻窦的RDD病理学特征在于:组织细胞吞噬淋巴细胞现象较为少见;增生的组织细胞可呈梭形,并可具有一定程度的异型性,呈模糊的旋涡状排列;在病变内淋巴管常扩张充满增生的组织细胞,淋巴管周围有淋巴组织包绕并可有反应性生发中心。本文中2例患者的病理结果均与以上特点相符,故结外鼻腔RDD诊断明确。结外型RDD临床表现多样,缺乏特征性表现,易误诊,鼻腔鼻窦的RDD可表现为鼻塞、脓涕、头痛、鼻出血等,需与鼻息肉、鼻腔内翻性乳头状瘤、恶性肿瘤、血管瘤、淋巴瘤、鼻硬结病等鉴别。其诊断主要依靠病理学检查确诊。本文报道的2例患者为起源于鼻中隔黏膜的结外RDD,均以反复鼻塞为主要症状,结合其体检及影像学资料,起初可能诊断为鼻息肉或鼻腔内翻性乳头状瘤,术前行病理学检查才得以确诊,对后续治疗方案的拟定具有重要意义。此外,RDD还可伴有发热、白细胞增多、血沉加快等,本文中2例患者均未出现发热,白细胞计数未见异常,未行血沉检查。对于RDD的治疗目前存在争议,尚无统一的治疗方法。RDD通常被认为是具有自限性的良性全身性疾病,预后较好,少数可自行消退,手术主要应用于危及生命或影响器官功能的病变(如上气道、中枢神经系统);而对于弥漫性渐进性病例,可以选择大剂量糖皮质激素、放疗、化疗、干扰素及单克隆抗体治疗。国内也见文献报道鼻腔鼻窦RDD行鼻内镜手术后口服泼尼松治疗,预防复发。本文2例患者均采用手术治疗,广泛切除了鼻腔内起源于鼻中隔黏膜的病变组织,以达到改善上气道通气的目的,术后未再给予药物治疗。2例患者术后半年复诊,恢复可,鼻腔通气良好,其远期疗效有待继续密切观察随访。
原始出处:
沈暘, 洪苏玲, 柯霞,等. 累及鼻中隔的Rosai-Dorfman病2例[J]. 临床耳鼻咽喉头颈外科杂志, 2017(9):718-720.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Rosai-Dorfman病#
66
#Dorfman#
92
#OSA#
64
#ROS#
80
#鼻中隔#
75
一起学习学习
111