肿瘤患者简明膳食自评工具的发明与研究
2019-04-20 丛明华 中华医学信息导报
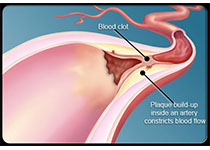
欧洲和北美的研究均证实,40%~60%的肿瘤患者存在程度不等的体重下降,其中,营养不良发生率30.9%。我国肿瘤营养不良流行病学调查研究显示超过50%的肿瘤患者存在营养不良。肿瘤患者食欲差、饮食量降低,并常伴有慢性炎症反应及代谢损伤,导致营养不良发生率明显高于其他慢性病。肿瘤患者出现体重下降或营养不良导致了较差的临床结局,包括治疗顺应性降低,副反应增加,生活质量下降,生存期缩短。因此肿瘤患者的营养
由于特殊的代谢特点及治疗相关的不良反应等原因,肿瘤患者常出现饮食量降低,导致营养不良发生率增高,并与较差的临床结局相关。前期研究发现,有一些患者的饮食量降低容易被患者自己及临床医护人员所忽视,需要进行膳食调查才能明确。而膳食调查需要专业的营养师完成,营养师又不能常规参与到临床工作中去,从而影响了这一技术的临床应用。作者在前期研究中发现,肿瘤患者的饮食模式有规律可循,依此规律将患者的饮食可以进行评分,从而快速了解患者饮食摄入量范围,为临床治疗的量化打下基础。
大部分患者的饮食情况符合以下5种模式:
简明特征描述
1分:三餐清流食,无肉、缺油
笔者开展了全国多中心横断面调查研究,纳入25家各地区医院,每个中心15例患者,使用NRS2002进行营养风险筛查,指导患者使用肿瘤患者简明膳食自评工具自我评价膳食评分,营养师做24 h膳食史回顾,评价患者具体能量及蛋白质摄入量。研究结果显示经过研究人员指导1~2次后患者进行饮食自评分,78%的患者的评分与营养师所做的24 h膳食回顾相吻合。绝大部分患者经过指导后可以理解自评表的含义,表明其具有可行性。该自评工具有待进一步验证其应用的临床意义,是否可以增加临床营养治疗的实施率以及是否可以协助改善肿瘤相关营养不良的发生。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#膳食#
76
#肿瘤患者#
59
谢谢了,学习
71
学习学习学习学习
80
1
79