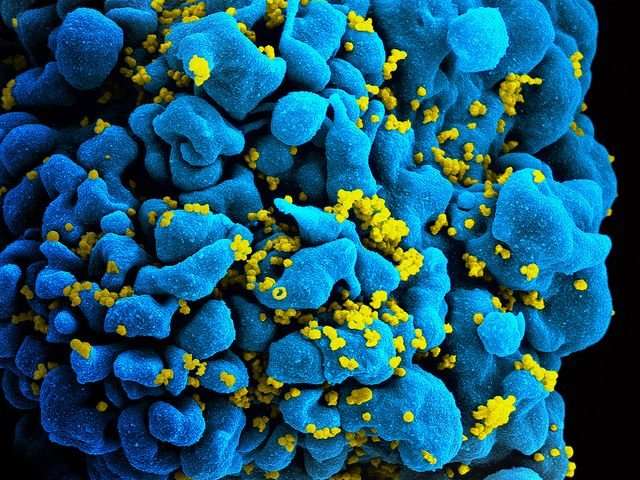
PLoS Pathog:科学家通过重建免疫系统有望将HIV彻底击败!
2017-10-13 sunshine2015 来宝网
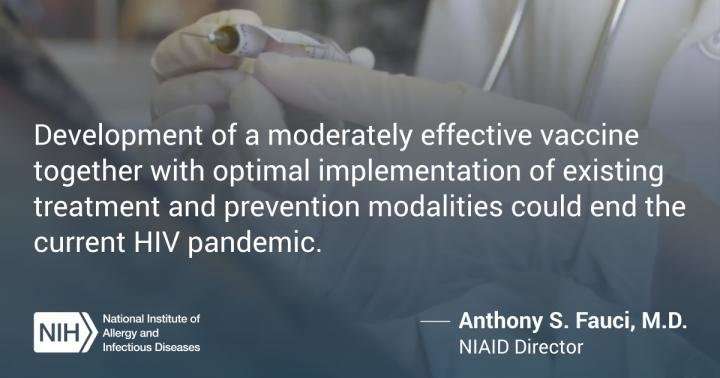
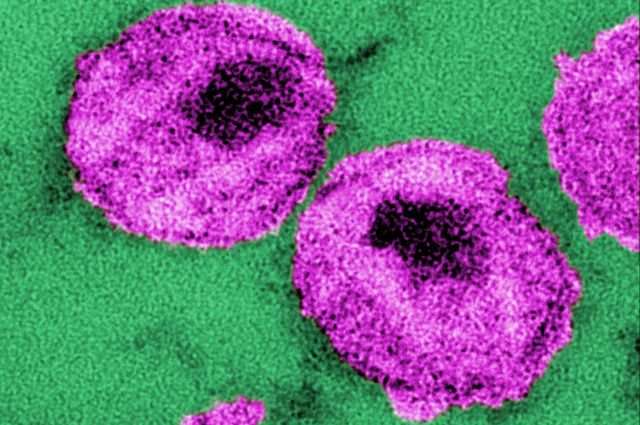
改进以前的尝试,科学家已经制定了一个新的策略,可能被用来重建病人本身的免疫系统细胞来对付艾滋病毒。在PLOS病原体中描述的方法在人细胞培养物和小鼠中显示出益处。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







学习一下很不错
111
学习
89
谢谢分享.有点意思
89
不错的.学习了.谢谢分享!
85
学习学习.了解了解
96
学习并分享!!
57
学习了
72
学习学习.继续关注
54