JCO:博来霉素、依托泊苷、顺铂的肺损伤影响有限
2016-02-27 zhaozhou 译 MedSci原创
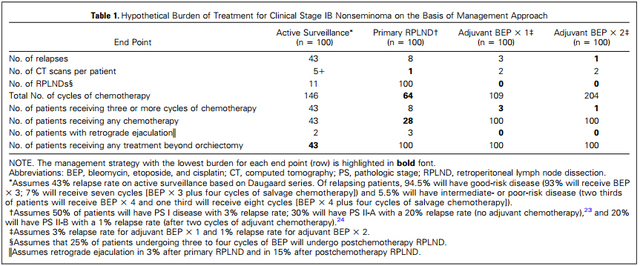
博来霉素最为人所知的不良反应是肺纤维化。使用博来霉素、依托泊苷和顺铂(BEP)治疗睾丸癌,患者由于博来霉素诱导的急性改变不高于6.8%,死亡风险为0-1%。使用BEP治疗生殖细胞癌症,有研究假设患者会有肺部毒性风险。因为前人的研究有着缺点,所以丹麦的研究人员开展了一项大规模的、非选择性的经过近期肺部功能监测的患者队列来进行研究,这些患者均是在使用BEP前后以及正在使用的时候接受监测,从
原始出处:
Jakob Lauritsen et al. Pulmonary Function in Patients With Germ Cell Cancer Treated With Bleomycin, Etoposide, and Cisplatin. JCO. Published Ahead of Print on February 22, 2016 as 10.1200/JCO.2015.64.8451
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#铂#
72
#JCO#
0
#博来霉素#
138
学习了科学一直在进步
215
#损伤#
77
#肺损伤#
70