J Gastroenterology H: 内镜胆道支架置入术是胆道狭窄患者超声内镜后胆管炎的危险因素
2021-05-30 MedSci原创 MedSci原创
胆道狭窄是由例如胰腺导管腺癌以及一些良性疾病导致的常见胆道疾病,在胆道癌患者中,超声内镜 (EUS)可以提供有关纵向/径向等癌症扩散、血管包裹和淋巴肿大的有用信息。
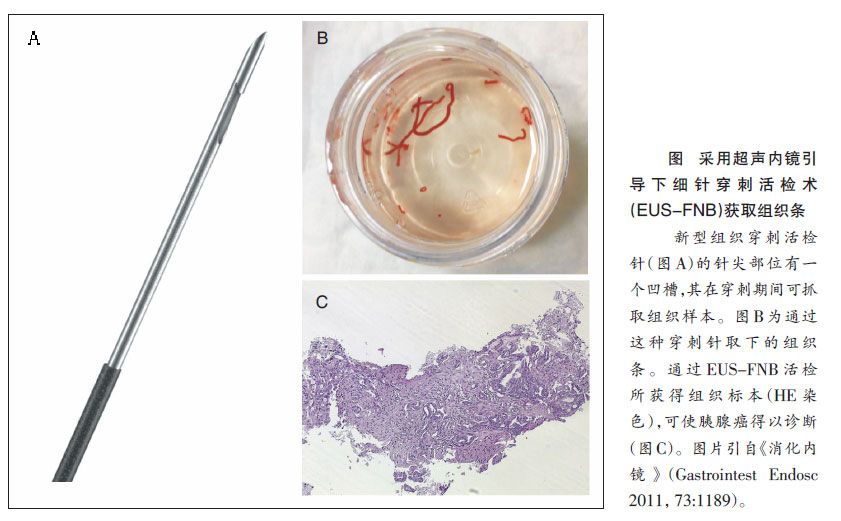
胆道狭窄是由例如胰腺导管腺癌以及一些良性疾病导致的常见胆道疾病,在胆道癌患者中,超声内镜 (EUS)可以提供有关纵向/径向等癌症扩散、血管包裹和淋巴肿大的有用信息。EUS 也有助于区分恶性和良性胆管狭窄。以EUS为基础的细针穿刺抽吸术 (EUS-FNA) 是一种常用的组织活检方法,EUS-FNA用于恶性胆道狭窄的诊断能力优于内窥镜逆行胰胆管造影 (ERCP)。但是,术后发生胆管炎的风险胆道疾病患者的 EUS/EUS-FNA没有得到充分研究,因此,本项研究旨在对此进行进一步分析。

研究人员回顾性收集了 2012 年 4 月至 2017 年 9 月接受 EUS/EUS-FNA 治疗的 136 例胆道狭窄住院患者,并评估了 EUS/EUS-FNA 后第二天发生并发症的情况。同时,为了研究的严谨性,研究人员排除了经皮胆道引流、难以到达十二指肠的患者以及同时接受内镜逆行胰胆管造影的患者。

本项回顾性研究共纳入了 121 名患者(147 例);90例为恶性。研究结果显示,已在 86 例中进行了内窥镜胆道支架置入术 (EBS) 的患者中,有 4.1% (6/147) 的患者中观察到 EUS 后发生了胆管炎的并发症,但是没有观察到其他与 EUS 相关的并发症。EBS合并胆管炎的发生率明显高于无EBS合并胆管炎的发生率(7.0% [6/86] vs 0% [0/61],P= 0.042)。胆汁酶升高也被确定为胆管炎的危险因素。
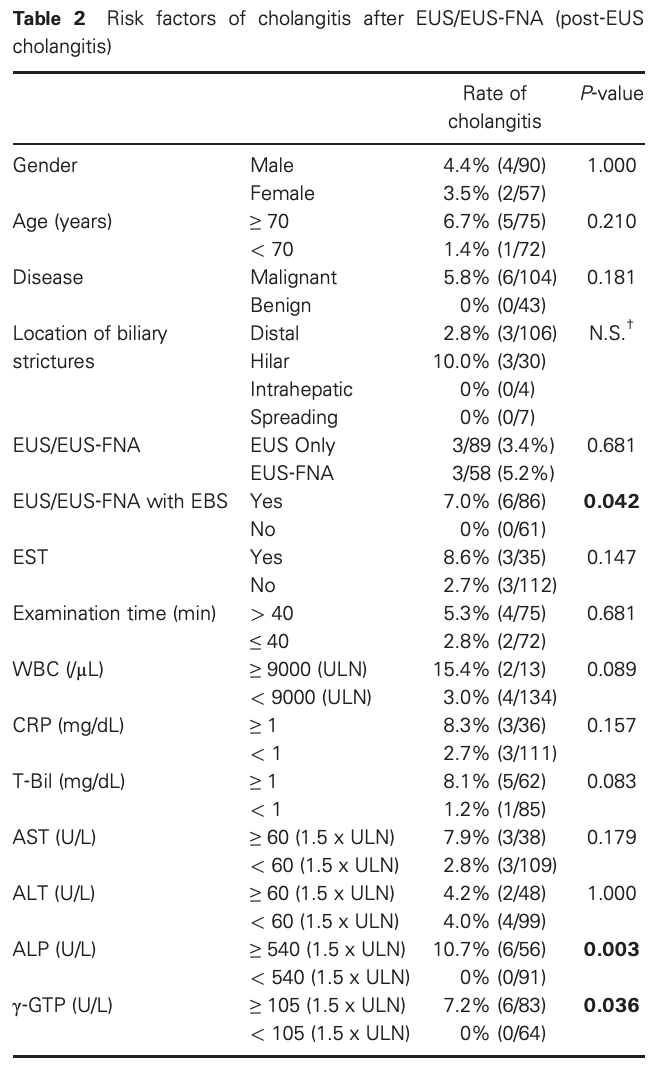
图:术后发生胆管炎的危险因素分析
本项研究通过回顾性分析证实内窥镜胆道支架植入术是与胆道狭窄患者 EUS 后胆管炎相关的危险因素。内镜医师应注意 EUS 术后胆管炎,尤其是 EBS 和胆汁酶升高的患者。
原始出处:
Kenji Ikezawa. Et al. Endoscopic biliary stenting as the risk factor for cholangitis after endoscopic ultrasound in patients with biliary strictures. Journal of Gastroenterology and Hepatology. 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#GAS#
120
#置入术#
81
#胆道支架#
64
#Gastroenterol#
84
#AST#
94
#内镜#
97
#Gastroenterology#
58
#胆管#
60
非常好的内容
102