J Am Coll Cardiol:这类心脏骤停患者成功复苏后的死亡风险仍高达90%!
2021-03-05 MedSci原创 MedSci原创
心脏骤停成功复苏后就安全了吗?
心脏骤停的死亡率居高不下。目前,院外心脏骤停(OHCA)的总体存活率约为10%。急性心肌梗死是OHCA的常见原因,约一半以上的心脏骤停幸存者至少存在一处心肌梗死。即使一开始就进行了复苏的患者,活着出院的概率也不过25%左右。
美国心脏病学会介入理事会发表了基于共识的建议,以帮助识别那些即使采用有创手术也不能提高存活率的临床特征不佳的接受复苏的心脏骤停患者。
本研究旨在明确可预测心脏骤停患者预后不良的临床特征。
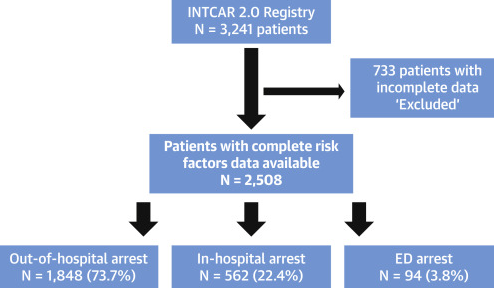
采用INTCAR(国际心脏骤停登记系统)来分别分析各种对生存不利的特征对心脏骤停患者活着出院的影响。
研究流程
在2508例心脏骤停后成功复苏的患者(正在进行的心肺复苏和非心脏病因被排除在外)中,发现了7个不利特征(总共10个)。终末期肾病被慢性肾病代替。
各种不利因素对患者活着出院的影响
总体上,39%的患者活到出院。影响患者活着出院的不良特征有:年龄>85岁(OR:0.30;95%CI:0.15~0.61)、恢复自主循环(ROSC)前的时间>30min(0.30;0.23~0.39)、非电击节律(0.39;0.29~0.54)、无旁观者心肺复苏(0.49;0.38~0.64)、乳酸>7mmol/l(0.50;0.40~0.63)、无目击停搏(0.58;0.44~0.78)、pH<7.2(0.78;0.63~0.98)和慢性肾病(0.96;0.70~1.33)。
不利特征数量与患者的存活率
任何3个或以上不利特征的存在都预示患者的存活率低于40%。3个影响最强的危险因素(年龄>85岁、ROSC前的时间>30min、非室性心动过速/室颤)或≥6不良特征的存在均预示患者活着出院的可能性不超过10%。
综上,心跳骤停复苏成功且有6个及以上不良特征的患者的远期预后较差。可考虑推迟甚至放弃对此类患者进行侵入性手术。
原始出处:
Harhash Ahmed A,May Teresa L,Hsu Chiu-Hsieh et al. Risk Stratification Among Survivors of Cardiac Arrest Considered for Coronary Angiography. J Am Coll Cardiol, 2021, 77: 360-371.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#Coll#
89
#Cardiol#
85
赞!
0
#死亡风险#
87
#复苏#
0
。
115
好文章!
111