Circulation:SGLT2抑制剂可降低2型糖尿病患者的高钾血症风险
2022-04-13 Nebula MedSci原创
SGLT2抑制剂可减少有高心血管风险的 2 型糖尿病患者的重度高钾血症风险,且不增加低钾血症风险
高钾血症会增加心律失常和死亡的风险,并限制肾素-血管紧张素-醛固酮系统 (RAAS) 抑制剂和盐皮质激素受体拮抗剂 (MRA) 的使用。钠-葡萄糖共转运蛋白 2 (SGLT2) 抑制剂可降低高心血管风险的 2 型糖尿病患者或慢性肾病(CKD)患者发生心肾事件的风险。但是,SGLT2抑制剂对高钾血症风险的影响尚不明确。
本研究是一项荟萃分析,对关于SGLT2抑制剂用于有高心血管风险的有无合并CKD的 2 型糖尿病患者的随机、双盲、安慰剂为对照的随机试验中常规监测了血钾水平的个人数据进行了分析。主要结果是发生重度高钾血症的时间,定义为中心实验室确定血清钾≥6.0 mmol/L,其他结果包括研究者报告的高钾血症和低钾血症(血清钾≤3.5 mmol/L)事件。
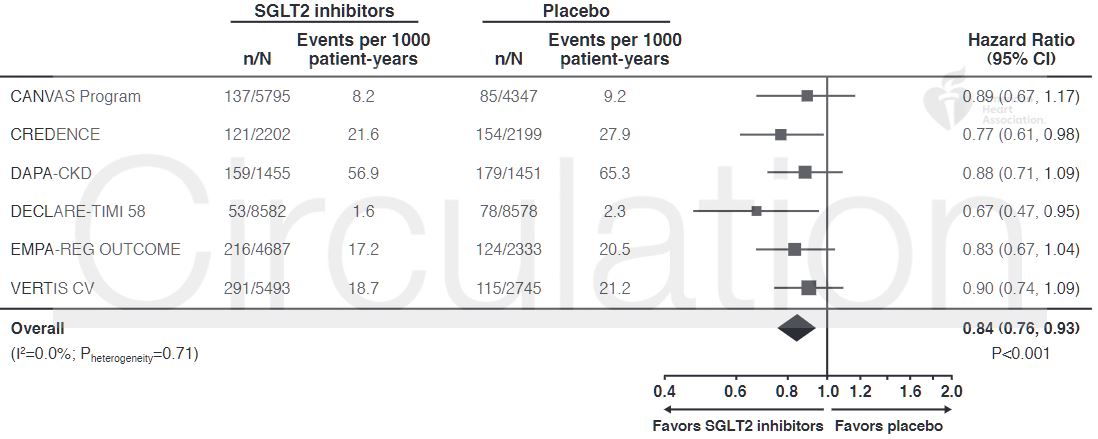
SGLT2抑制剂对重度高钾血症风险的影响
经筛查,有6项临床试验符合纳入标准,共包含49875位受试者,评估了4种SGLT2抑制剂。1754位受试者发生过重度高钾血症,另外1119位记录了研究者报告的高钾血症事件。SGLT2抑制剂可降低重度高钾血症的风险(HR 0.84),该效果在各个研究中一致(p异质性=0.71)。服用 SGLT2 抑制剂的受试者研究者报告的高钾血症发生率也较低(HR 0.80, p异质性=0.21)。
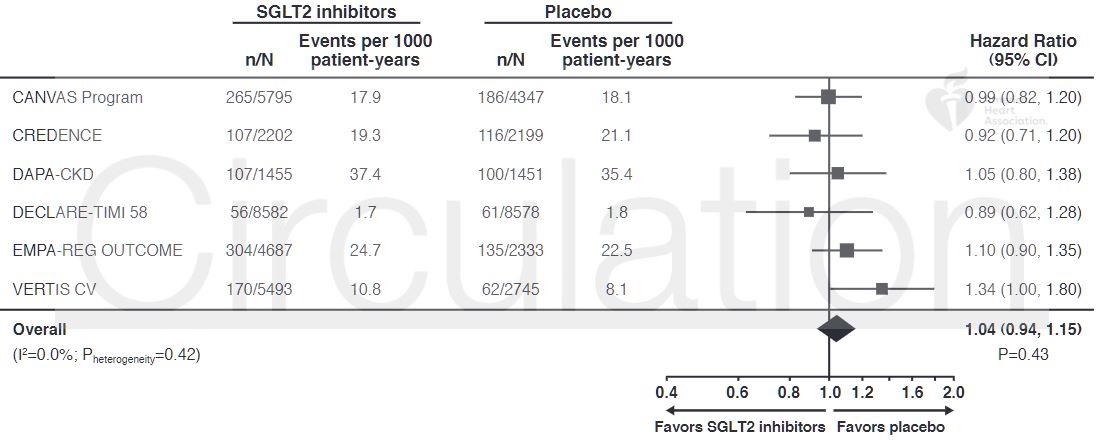
SGLT2抑制剂对低钾血症风险的影响
此外,研究人员在一系列亚组(包括基础肾功能、心衰史、RAAS抑制剂、利尿剂和MRA使用)分析中都观察到重度高钾血症的减少。最后,SGLT2抑制剂不增加低钾血症风险(HR 1.04, p异质性=0.42)。
综上,SGLT2抑制剂的使用可减少有高心血管风险的 2 型糖尿病患者(无论有无合并慢性肾病)的重度高钾血症风险,且不增加低钾血症风险。
原始出处:
Neuen Brendon L,Oshima Megumi,Agarwal Rajiv et al. Sodium-glucose Cotransporter 2 Inhibitors and Risk of Hyperkalemia in People with Type 2 diabetes: A Meta-analysis of Individual Participant Data from Randomized Controlled Trials.[J] .Circulation, 2022, https://doi.org/10.1161/CIRCULATIONAHA.121.057736.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#2抑制剂#
94
#SGLT#
76
#抑制剂#
55
SGLT2-i越来越多发现!
124
学习了
120
#2型糖尿病患者#
73
#糖尿病患者#
42
#SGLT2#
71
#高钾#
69