JAHA:他汀类药物降低低密度脂蛋白胆固醇能让中年人重获得低风险保护吗?
2021-05-17 MedSci原创 MedSci原创
接受他汀类药物治疗且LDL-C<100 mg/dL的个体与未经治疗且LDL-C<100mg/dL的个体发生动脉粥样硬化性CVD的风险水平相似。
目前尚不清楚中年期开始接受他汀类药物治疗能否逆转高胆固醇血症患者的心血管风险。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,在基线时,研究人员根据他汀类药物的治疗建议和他汀类药物的治疗状态,将5687名50岁以上且无临床心血管疾病(CVD)的动脉粥样硬化多种族研究(MESA)的参与者进行分组。

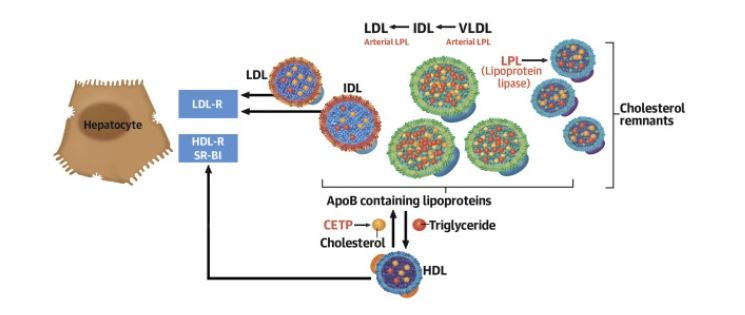
研究人员使用Cox回归比较了未经治疗的低密度脂蛋白胆固醇(LDL-C)<100 mg/dL(对照)组与其他组之间的冠心病和CVD风险,并调整了CVD危险因素。研究人员还根据LDL-C水平(<或≥100mg/dL)、冠状动脉钙化评分(0或>0 Agatston单位)和他汀类治疗状态(未治疗或已治疗)将参与者进行分组,其中未经治疗且LDL-C<100 mg/dL以及冠状动脉钙化评分=0 Agatston单位作为对照组。

LDL-C与CVD
在15年的随访期间,共发生了567例冠心病和848例CVD事件。接受他汀类药物治疗的LDL-C<100 mg/dL组冠心病和CVD风险比(HRs)分比为1.16(95%CI为0.85-1.58)和1.02(95%CI未0.78-1.32)。但是,接受他汀类药物治疗且LDL-C<100 mg/dL以及冠状动脉钙化评分>0 Agatston单位的参与者,冠心病的HR为2.6(95%CI为1.7-4.2),而CVD的HR为1.8(95%CI为1.2-2.6)。
由此可见,接受他汀类药物治疗且LDL-C<100 mg/dL的个体与未经治疗且LDL-C<100mg/dL的个体发生动脉粥样硬化性CVD的风险水平相似。但是,尽管进行了降脂治疗,但冠状动脉钙化评分>0 Agatston单位的个体仍具有较高的风险,这表明在中年期开始他汀类药物治疗可能无法重塑冠状动脉粥样硬化一级预防的低危状态。
原始出处:
Kiang Liu.et al.Does Lowering Low‐Density Lipoprotein Cholesterol With Statin Restore Low Risk in Middle‐Aged Adults? Analysis of the Observational MESA Study.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/10.1161/JAHA.120.019695
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#他汀类药#
78
#AHA#
0
#脂蛋白#
59
#中年人#
78