1
门诊来了位棘手的病人
病例摘要
患者姚某,女性,49岁,主因持续性肢体麻木2年,加重伴腹泻、乏力20天入院。患者2年前无明显诱因开始出现肢体麻木、乏力,偶伴腹泻。入神经内科就诊后,诊断为神经症,口服抗焦虑药物治疗后症状无改善。2年来肢体麻木持续存在,并频繁发作腹泻,每月1~2次,每次2~3天。20天前再次出现腹泻,4天前开始出现四肢软瘫。
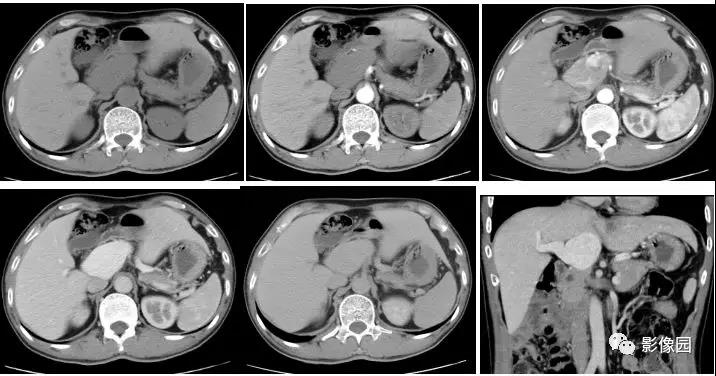
入当地医院就诊后检查提示血钾2.88mmol/L,血钙1.07mmol/L,血氯97.0mmol/L,钠138mmol/L,pH7.51,头颅CT提示双侧苍白球钙化。予补钾补钙后症状好转。但出院后再次出现类似症状,遂入我院就诊。
图1 头颅CT提示苍白球钙化
这个病例不太寻常,大家从来没有见过这样奇特的临床表现。一时间,科室里的医生都有点拿不定主意,众说纷纭,但下什么诊断好像都不够准确,连临床经验丰富的主任也似乎被难住了。时间紧迫,看着病床上痛苦不堪的患者,我们需要尽快找到谜底……
2
抽丝剥茧,逼近真相
低钙病因有很多种,包括摄入不足、排泄增加和异常转运等。但是低钙伴异位钙化灶,应首先考虑钙磷代谢相关激素的紊乱。
基于此,我们检查了患者的甲状旁腺功能。两次复查甲状旁腺激素,分别为0.0pg/mL和5.7pg/mL,远低于正常范围(12~88pg/mL)。甲状旁腺SPECT未见甲状旁腺显像。骨密度检查提示患者骨密度异常增高。
甲状旁腺激素抑制成骨作用,降钙素正好相反,二者的平衡是维持血钙正常的关键。降钙素的作用占据优势时,成骨作用加强,血钙就会异常降低,同时伴有异位钙化。至此,我们可以初步诊断:该患者由于甲状旁腺机能减退而引起钙磷代谢紊乱,导致钙离子异常沉积,血钙降低。
但是,低钾的原因如何解释?
患者入院继续出现腹泻症状,每日排便4~7次。持续静脉补钾、补钙后,血钾、血钙回升不明显,血钾波动在2.6~3.3mmol/L之间,血钙波动在0.99~1.42mmol/L之间。血气分析提示pH波动在7.45~7.51之间。
低钾的原因同样多种,包括摄入不足、丢失增加(经胃肠道或经肾脏)、向细胞内转运等。血钙降低可以导致胃肠道平滑肌痉挛,导致患者出现难治性腹泻,这可能是引起低钾血症的原因。结合患者出现碱中毒的表现,我们将低钾暂时归因为低钙导致的腹泻所致。
然而事实果真如此吗?
患者无高血压病史,入院后血压波动在85~105/55~70mmHg之间。肾上腺CT提示:双侧肾上腺未见明显异常。皮质醇、ACTH节律正常,卧位醛固酮14.0ng/dL(正常值5.9~17.4),立位醛固酮22.0ng/dL(6.5~29.6),卧位肾素4.51ng/mL(0.05~0.79),立位肾素12.79ng/mL(0.93~6.56)。24小时尿量1550mL,尿钾27.7mmo/L,尿钾总量43mmol,尿pH6.5。当日血钾3.2mmol/L。
患者血钾降低,尿钾却异常增加,并且出现高肾素血症,令人困惑。如果该患者是由于平滑肌痉挛引起的腹泻导致胃肠道排钾增加,尿钾量应大量减少。一元论已无法解释低钾和低钙同时出现,需要考虑并存其他疾病。
3
最可能的谜底
尿钾增加的疾病包括以下几种:
1. 原发性醛固酮增多症:患者可出现高血压、低血钾的症状,但该患者血压一直偏低;
2. 肾小管酸中毒:患者可出现碱性尿、酸中毒,但该患者血气分析一直提示为碱中毒,尿pH不高;
3. Liddle综合征:同样也应表现为低血钾,碱性尿,与该患者不符;
4. Gitelman综合征和Bartter综合征:表现为低血压、低血钾、高肾素,与本患者症状相符。因此,应考虑该患者同时患有Bartter综合征。
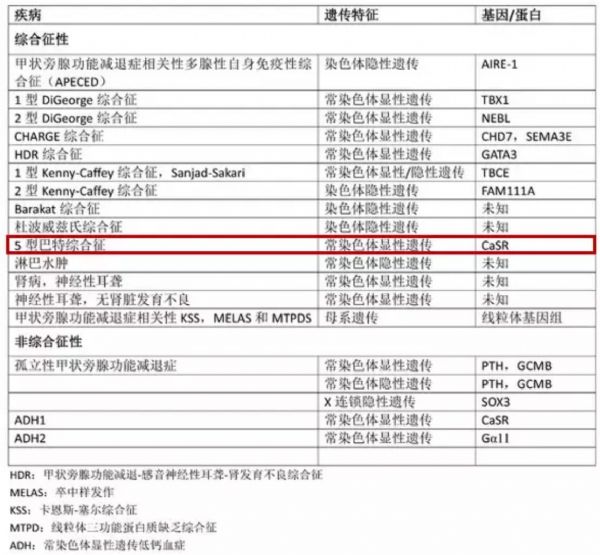
Bartter综合征是一组常染色体突变遗传病,其特征是肾小管Henle袢升支粗段盐的转运明显减少,根据基因突变类型可分为6型,Gitelman综合征是其中一种亚型。V型Bartter综合征为钙敏感受体(CaSR)功能获得性突变所致轻度失盐性肾小管疾病。
甲状旁腺功能减退可表现为孤立型和综合征型,均为基因突变引起的遗传性疾病。CaSR功能获得性突变同样可引起甲状旁腺功能低下及低钙血症。
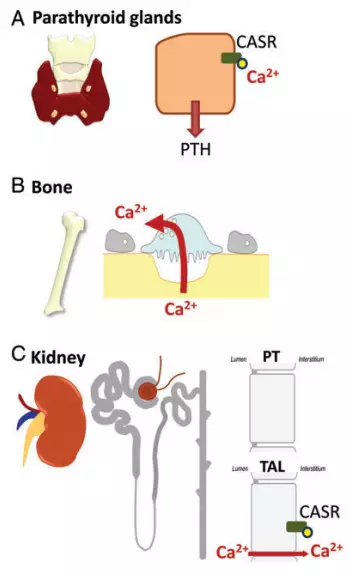
图2 钙敏感受体在组织中的表达。A.在甲状旁腺中表达,影响甲状旁腺激素分泌;B. 甲状旁腺激素继而影响成骨过程及血钙浓度;C.在肾小管中表达,影响肾小管离子分泌。
因此,该患者应考虑为CaSR功能获得性突变同时引起甲状旁腺功能减低及Bartter综合征,这两种疾病分别引起了顽固的低钙血症和低钾血症。低钾和低钙终于能用一元论完美解释了。
图3 甲状旁腺功能减退症相关性遗传疾病
较为遗憾的是,该患者因经济原因未行基因学检测,未能证实是否发生CaSR功能获得性突变。因此,其诊断仍有可供商榷之处。在这个柳暗花明的诊断过程中,我们一直试图用一元论解释临床现象,最终找到了合理的解释。
原始出处:
1. Ogo Egbuna, Edward Brown. Hypercalcaemic and hypocalcaemicconditions due to calcium-sensing receptor mutations. Best Pract Res ClinRheumatol. 2008; 22(1): 129–148.
2. Bart Clarke et al. Epidemiology and Diagnosis of Hypoparathyroidism.J Clin Endocrinol Metab. 2016 Jun; 101(6): 2284–2299.
3. Walsh PR et al. Clinical and diagnostic features of Bartter and Gitelman syndromes. Clin Kidney J. 2018 Jun; 11(3):302-309.
4. Bonny O et al. Genetics of calcium homeostasis in humans: continuumbetween monogenic diseases and continuous phenotypes. Nephrol Dial Transplant. 2014 Sep; 29 Suppl 4:iv55-62.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#罕见病例#
107
学习了,谢谢分享
90
#罕见#
71
已学习并已分享
100
遇到每一个病人都需要我们认真对待和思考。
96
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
92