外阴颗粒细胞瘤 1 例
2019-06-11 卢烨 石洪爽 武 昕 现代妇产科进展
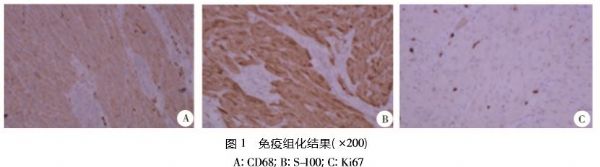
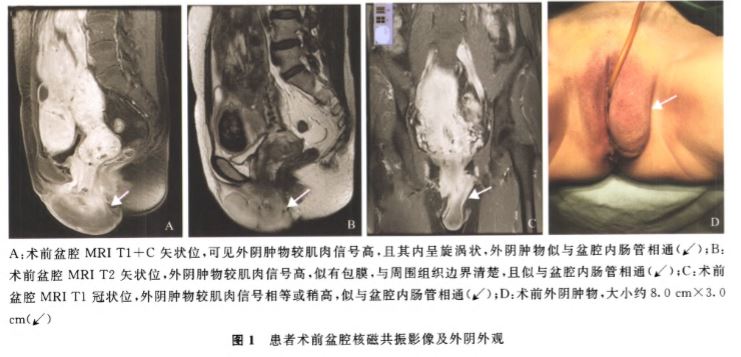
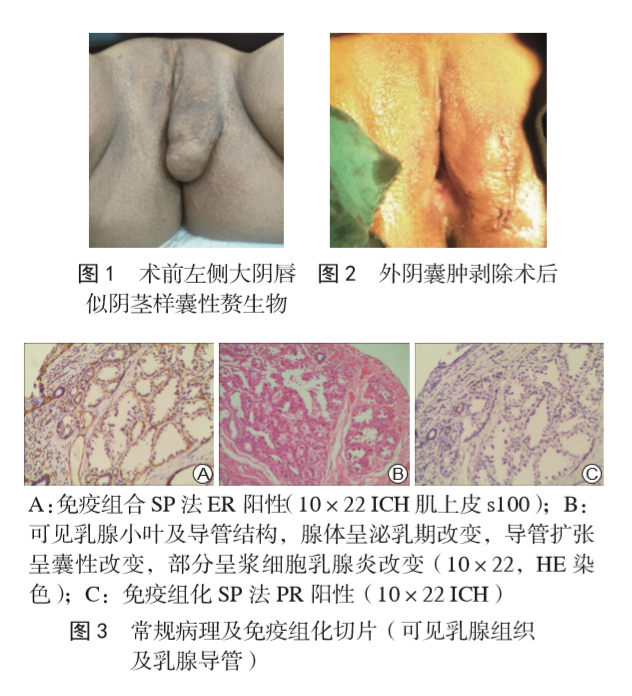
患者, 女, 26岁, 以“发现外阴肿物2 年”于2018 年10 月就 诊于我院。患者2年前于右侧小阴唇上方触及1cm左右质硬肿 物,无痛,不痒,未就诊,肿物未见明显增大,现因局部不适感来 诊。患者在门诊行外阴病灶活检,病理回报:颗粒细胞瘤。查 体:双侧腹股沟未触及肿大淋巴结。妇科检查:外阴发育正常; 右侧小阴唇上方,靠近阴蒂部位,可见粉白色外生的质硬结节,直径约1.5cm,界限清楚,基底部活动
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








了解一下
87
了解一下
86
了解一下
96
#细胞瘤#
51
#颗粒细胞瘤#
63