Nature:科学家揭秘常见脑血管疾病的发病机制
2016-04-05 佚名 生物谷
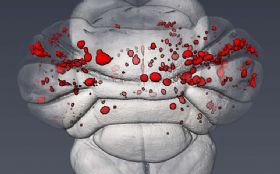
大脑海绵状血管畸形(CCMs)是大脑中薄壁血管膨胀的一种集群形式,其会引发中风和癫痫发作,然而具体发病机制目前研究者尚不清楚;近日来自宾夕法尼亚大学的研究人员通过研究发现了隐藏在这种脑血管疾病发生背后的一种新型的分子机制,相关研究刊登于Nature杂志上。 通常在100至200人中会有一名大脑海绵状血管畸形患者,该疾病主要表现为两种方式,第一种是散发状态,占到了80%的患者,另外一种则是遗传性
大脑海绵状血管畸形(CCMs)是大脑中薄壁血管膨胀的一种集群形式,其会引发中风和癫痫发作,然而具体发病机制目前研究者尚不清楚;近日来自宾夕法尼亚大学的研究人员通过研究发现了隐藏在这种脑血管疾病发生背后的一种新型的分子机制,相关研究刊登于Nature杂志上。
通常在100至200人中会有一名大脑海绵状血管畸形患者,该疾病主要表现为两种方式,第一种是散发状态,占到了80%的患者,另外一种则是遗传性的病例。本文研究中研究人员调查了是否一种特殊保守性的机制是引发患者出生后大脑发生CCMs的原因,利用CCM疾病的新生小鼠模型,研究者发现,在小鼠机体中新形成的CCM损伤处酶类MEKK3的靶点基因,KLF2和KLF4的表达水平增加了。同时MEKK3靶点基因,KLF2和KLF4的特异性缺失还会完全恢复小鼠机体中的患处,并且抑制小鼠因CCM疾病而死亡。
同时研究者还发现,在人类家族性和散发性的CCM疾病患者机体的血管内膜细胞中,基因KLF2和KLF4的表达水平提高了;而且MEKK3信号通路的增加及KLF2和KLF4转录因子过表达水平的上升就是CCM发生的根本原因,由KLFs是MEKK3的靶点,因此较高的MEKK3活性就意味着KLF基因表达水平的增加。
家族性及散发性CCMs的发生或许都是由于内皮细胞中MEKK3-KLF2/4信号的产生而致,而这对于开发新型疗法阻断这些蛋白的活性提供了新的思路,此外研究者Kahn目前也正在调查那种KLF2/4靶点基因主要负责产生CCM患者机体的损伤,一项在发育心脏中进行的平行研究中研究者揭示了ADAMTS酶类的关键角色,ADAMTS可以帮助降解一种多能聚糖,这种多能聚糖是和CCM相关的一种特殊物质,其在大脑中高水平表达。
最后研究者表示,我们发现了早期CCM患者机体患处中多能聚糖的降解现象,这对于我们理解CCM的病理学机制以及后期寻找潜在的治疗性靶点提供了新的思路和希望。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
52
#脑血管疾病#
63
#血管疾病#
68
标题党,内容不丰富嘛。
106
()
145
写……
105
发病机制
127