JAMA:IL-23 抑制剂Risankizumab 对中度至重度银屑病患者治疗结果的影响
2021-09-03 医路坦克 MedSci原创
斑块状银屑病是一种慢性免疫介导的全身性疾病,其特征厚厚的皮肤上覆盖着干燥和银色鳞屑(斑块),通常伴有灼烧感、瘙痒和疼痛。斑块的外观表现经常导致患者心理困扰。
Risankizumab (ABBV-066) 是一种抗 IL-23 单克隆抗体药物,目前,原研艾伯维正在进行研究其用于治疗多种炎症性疾病,包括银屑病、克罗恩病、溃疡性结肠炎、特应性皮炎和银屑病关节炎。
斑块状银屑病是一种慢性免疫介导的全身性疾病,其特征厚厚的皮肤上覆盖着干燥和银色鳞屑(斑块),通常伴有灼烧感、瘙痒和疼痛。斑块的外观表现经常导致患者心理困扰。其身体和心理社会负担会严重损害社会功能、工作和日常活动以及健康—许多银屑病患者的相关生活质量 (HRQL),
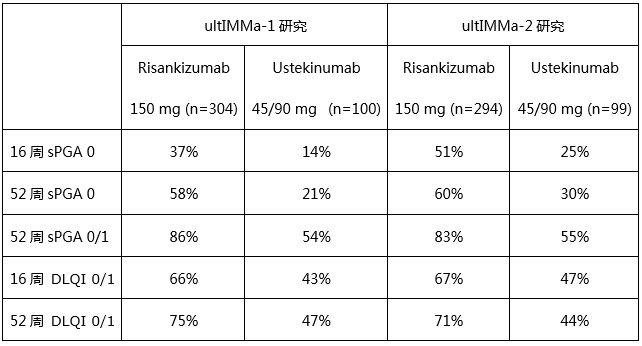
Risankizumab 是一种白细胞介素 (IL)-23 抑制剂,是一种在美国和欧洲获得批准的新型人源化 IgG1 单克隆抗体。两个3期重复临床试验证明,Risankizumab 优于 IL-12/23 抑制剂乌司奴单抗,同时保持与优特克单抗相似的良好安全性。第 16 周的皮肤病生活质量指数 (DLQI) 和银屑病症状量表 (PSS) 被列为次要终点。本研究在这2个3期试验中通过 PRO 从患者的角度报告了一段时间内的治疗效果。
UltIMMa-1 和 UltIMMa-2 研究是重复的 52 周第 3 期、随机、多中心、双盲、安慰剂对照和活性对照药对照试验,分别在在亚太、日本、欧洲和北美的全球 139 个站点(包括医院、学术医疗中心、临床研究单位和私人诊所)。患有中度至重度慢性斑块状银屑病且体表面积 (BSA) 占 10% 或更多、银屑病面积严重程度指数 (PASI) 得分为 12 或更高、静态医师总体评估 (sPGA) 得分为 3 的成人(18 岁)或更高的都包括在内。
干预:在每项试验中,患者被随机分配 (3:1:1) 接受 150 mg Risankizumab、45 mg 或 90 mg 优特克单抗(每个标签基于体重)52 周,或匹配安慰剂 16 周,然后是 Risankizumab。
主要结果和测量:来自 2 项试验的综合数据用于比较银屑病症状量表 (PSS)(疼痛、发红、发痒和灼痛的总分和项目评分) )、皮肤科生活质量指数 (DLQI)、5 级 EuroQoL-5D (EQ-5D-5L) 和医院焦虑和抑郁量表 (HADS),开始、第 16 周和第 52 周。
结果:共分析了 997 名中度至重度慢性斑块状银屑病患者。在所有组中,平均年龄为 47.2 至 47.8 岁,68.3%(优特克单抗为 136/199)至 73.0%(安慰剂为 146/200)为男性。基线时所有治疗组的患者特征和 PRO 具有可比性(Risankizumab、Ustekinumab 和安慰剂分别为 n = 598、199、200)。在第 16 周,与使用优特克单抗或安慰剂治疗的患者相比,接受 Risankizumab 治疗的患者达到 PSS = 0 的比例显着更高,表明没有银屑病症状(30.3% [181/598]、15.1% [30/199]、1.0% [2] /200],两者 P<.001),DLQI = 0 或 1 表示对皮肤相关 HRQL 没有影响(66.2%、44.7%、6.0%,P<.001)。与优特克单抗或安慰剂相比,接受 Risankizumab 治疗的患者在 DLQI 方面达到最小临床重要差异 (MCID) 的比例显着更高(94.5% [516/546]、85.1% [149/175]、35.6% [64/180];两者 P< . 001)、EQ-5D-5L(41.7% [249/597] 对 31.5% [62/197],P= .01;对 19.0% [38/200],P< .001)和 HADS(焦虑: 69.1% [381/551] vs 57.1% [104/182],P= .004;vs 35.9% [66/184],P< .001;抑郁:71.1% [354/598] vs 60.4% [96/ 159],P= .01;对比 37.1% [59/159],P< .001)。在第 52 周时,与使用优特克单抗治疗的患者相比,接受 Risankizumab 治疗的患者在 PSS、DLQI 和 EQ-5D-5L 方面的改善持续。
结论和相关性
Risankizumab 显着改善了中度至重度银屑病的症状,与优特克单抗或安慰剂相比,改善了 HRQL,并减少了心理困扰。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#中度至重度#
79
#mAb#
59
#IL-23#
106
#治疗结果#
80
#IL-2#
64
#抑制剂#
69
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
107
#risankizumab##银屑病#
176