Calcif Tissue Int:老年女性的骨转换标志物特征与骨折风险:75岁至90岁的骨折风险
2022-09-08 医路坦克 MedSci原创
骨质疏松性骨折是临床医疗中的一个相当大的问题,目的是调查两个IOF推荐的BTM,以及其他四个反映骨转换不同方面的BTM,确定BTMS与特定骨折部位的相关性,时间对风险预测的影响,以及评估时年龄的影响。

骨质疏松性骨折是临床医疗中的一个相当大的问题,因为它对患者和临床医疗造成了负担;此外,随着人口老龄化,这一数字将增加。一项重大挑战是正确识别脆性骨折的高危人群。错乱的骨转换/重建导致结构改变,骨密度降低,骨强度降低,最终导致骨折。骨转换可以通过在重塑过程中释放的蛋白质或蛋白质片段来评估。通常,骨形成和骨吸收是耦合的,从这两个过程中释放的骨转换标志物(BTM)反映了整体的骨转换。
多年来,许多用于骨吸收和形成的标志物已经被评估与骨丢失、骨折风险和药物疗效有关。这些标记物捕捉了骨代谢的不同方面,对于我们理解骨转换是必不可少的,包括对于骨吸收,C端交联型I型胶原端肽(CTX)和抗酒石酸酸性磷酸酶5b(TRAcP5b),分别作为胶原降解和破骨细胞活性的指标。对于骨形成,标志物包括I型胶原N末端前肽(PINP)作为胶原形成的指示物,骨特异性碱性磷酸酶(BALP)指示成骨细胞的活动和潜在的矿化,最后是骨钙素,成骨细胞分泌的非胶原蛋白和骨转换的替代标志物。此外,尿骨钙素碎片(U-OC)可能起源于骨吸收或形成,最有可能反映整体骨转换,已经进行了评估。国际骨质疏松基金会(IOF)和国际临床化学联合会(IFCC)推荐了两种用于研究和监测治疗的参考标记物,CTX和PINP。Meta分析证实,这些标志物的高水平与骨折风险增加之间存在显著的关联。
虽然现有研究已经推进了有关骨转换标志物作为骨折治疗工具的作用的文献,但我们对BTM和骨折风险之间的联系的理解仍然存在差距,特别是在骨折最常见的老年女性中,部分原因是研究设计和报告的异质性。本研究是在预期的、基于人群的OPRA女性队列中进行的,她们都在纳入时年龄为75岁,在80岁和85岁时重新调查,并以15年的视角观察骨折数据。目的是调查两个IOF推荐的BTM,以及其他四个反映骨转换不同方面的BTM,确定BTMS与特定骨折部位的相关性,时间对风险预测的影响,以及评估时年龄的影响。
方法:以人群为基础的OPRA队列(n=1044)在75岁、80岁、85岁和骨折记录长达15年时进行评估。每个时间点检测6种骨钙素(I型胶原N端肽,PINP;总骨钙素,OC;骨特异性碱性磷酸酶,BALP;I型胶原C端肽,CTX;抗酒石酸酸性磷酸酶5b,TRAcP5b;尿骨钙素)。根据短期(1、2、3年)和长期风险(5、10、15年)计算任何严重骨质疏松性、椎体和髋部骨折的风险比(HR)。
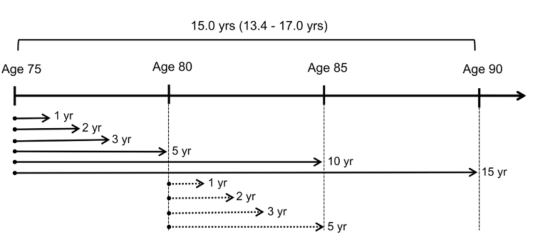
在OPRA队列分析中,首先使用基线(75岁)时测量的BTM,然后在80岁时测量BTM,以确定BTM对骨折预测的分析框架。裂缝预测被评估为“短期风险”(1年、2年或3年)和“长期风险”(5年、10年或15年)。
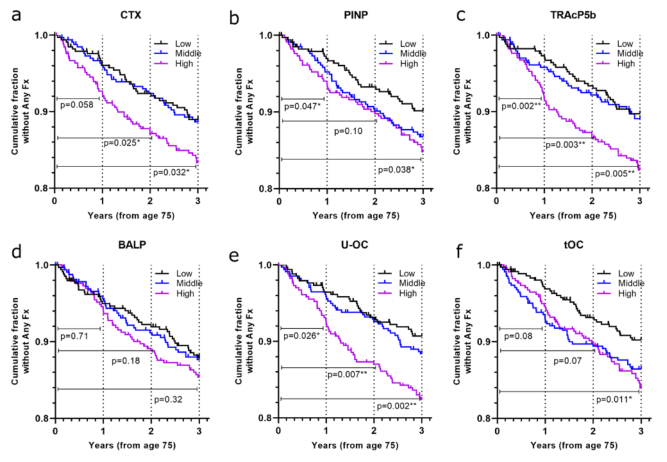
在75岁时使用BTMS测量的任何骨折的短期骨折风险。未发生任何骨折的女性的累积比例呈Kaplan-Meier曲线,分别为a CTX、b PINP、c TRAcP5b、d BALP e U-OC f TOC。三分色分为低(黑色)、中(蓝色)和高(洋红色)。报告了1年、2年和3年的P值(对数等级检验)(地砖低与高,未调整)。终点是第一次骨折的日期(如果没有骨折,则为随访时间的结束)和死亡日期。并与没有骨折的女性进行了比较。一年结束时有骨折的女性人数为51人,两岁时(93人),三岁时(130人)
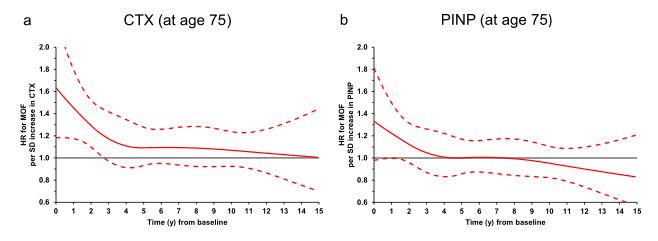
严重骨质疏松性骨折的危险比(HR)。为了模拟BTMS随时间变化的预测价值,使用修正的泊松回归模型分析了MOF风险(BTMS中每SD变化的心率),对75岁时测量的CTX和b PINP进行了修正,调整了基线吸烟、双磷酸盐使用、既往骨质疏松性骨折的情况。实线代表人力资源;虚线代表95%的顺位
结果:在75岁时,在大多数时间范围内,高CTX水平与所有骨折的风险增加相关,包括主要的骨质疏松性骨折(比率范围:1.28至2.28)。PINP并不总是与之相关。尿骨钙素一直与增加的短期风险相关(相对危险度范围:1.83-2.72)。其他BTM在方向性上是一致的,尽管不是所有的统计意义上都是显著的。BTM不能预测髋部骨折。所有BTM的相关性随着时间的推移而减弱;在80岁时,没有一个与增加骨折风险相关。
结论:CTX、尿OC和TRAcP5b对1~3年内骨折有预测作用,而在80岁以上的远期患者中,BTMS的预测价值较低。在高龄患者中,吸收标记物,尤其是环磷酰胺,与骨折风险的相关性比形成标记物更一致。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#转换标志物#
73
#标志物#
84
#Tissue#
82
#骨转换标志物#
73
CTX在最后错❌写成环磷酰胺
70
#骨折风险#
94