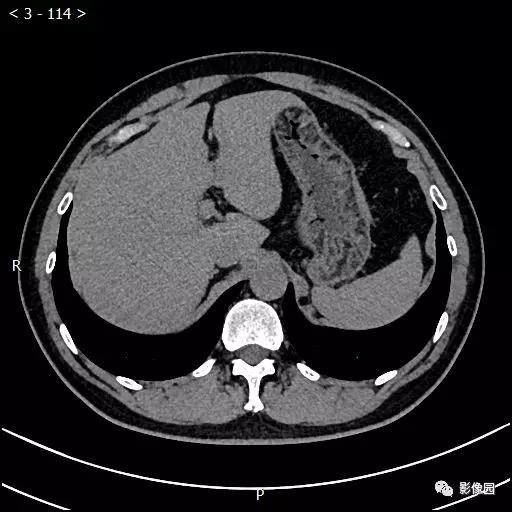
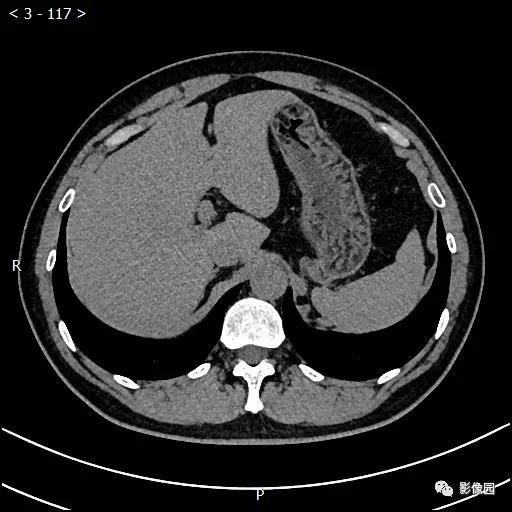
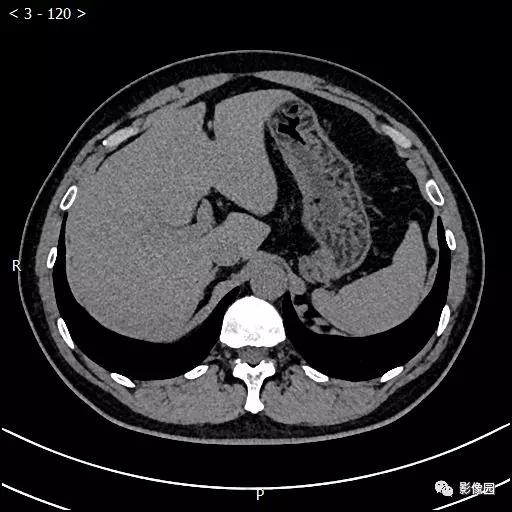
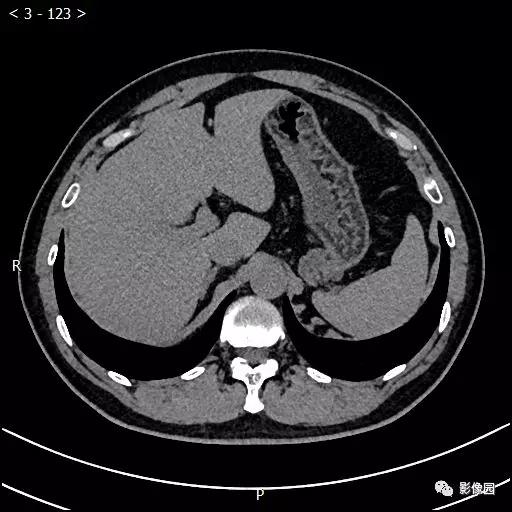
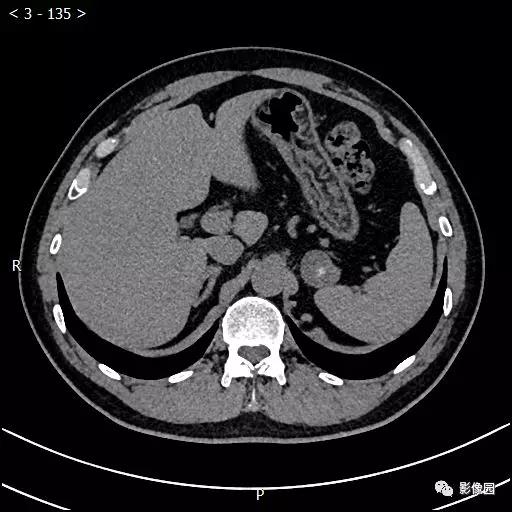
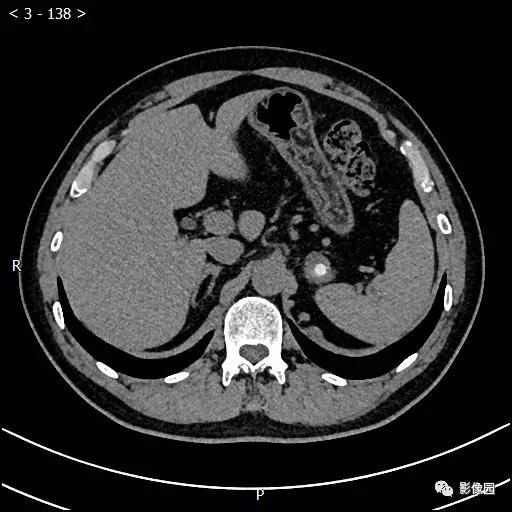
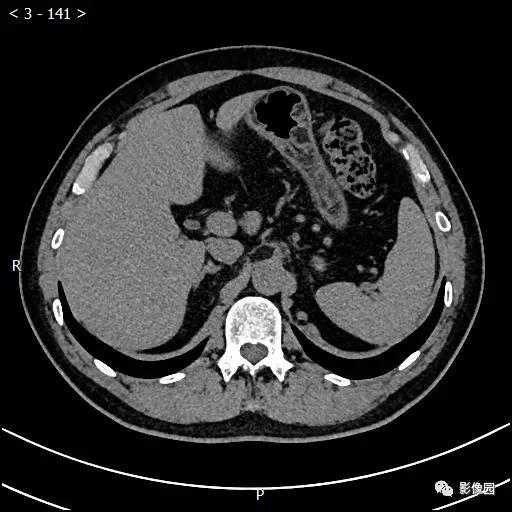
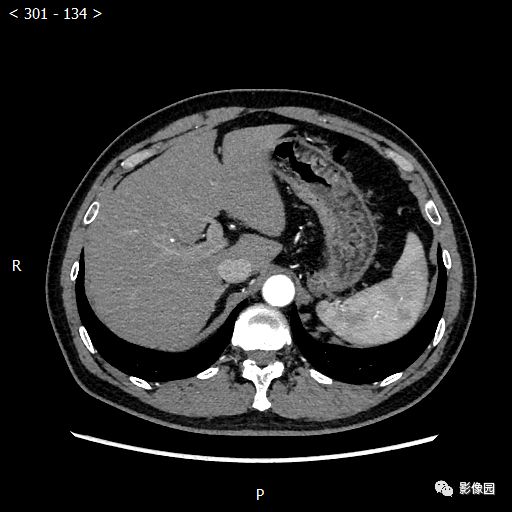
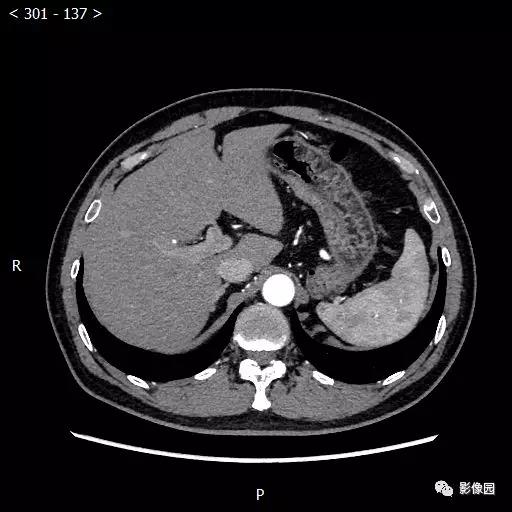
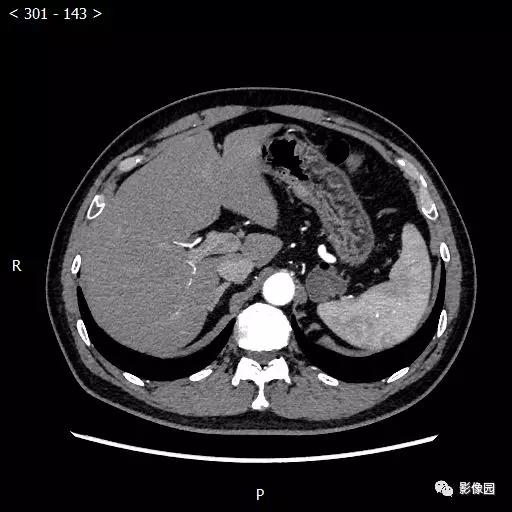
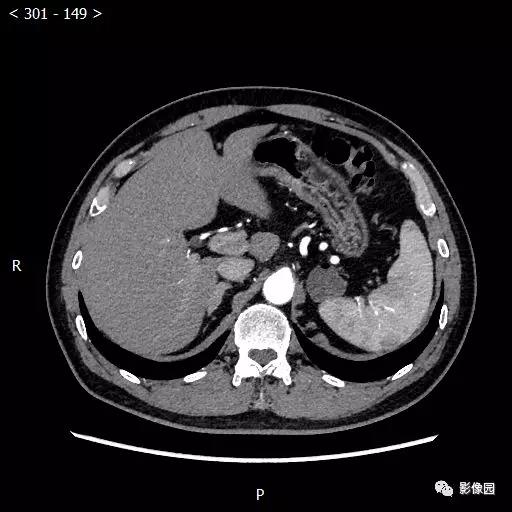
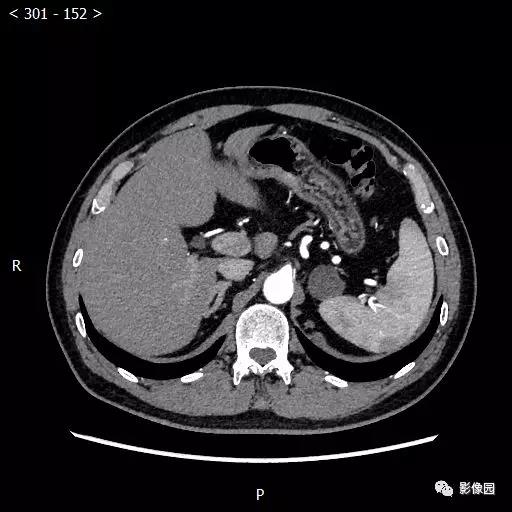
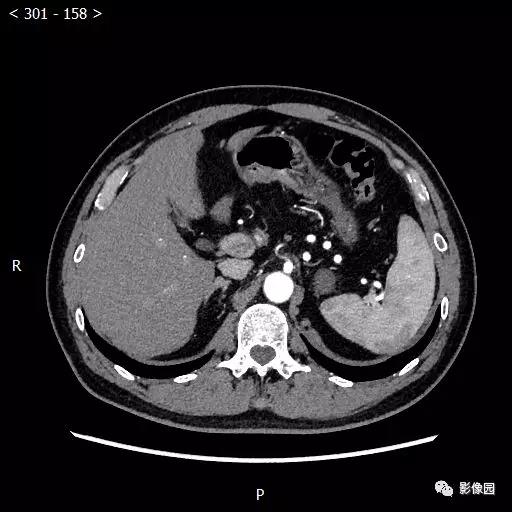
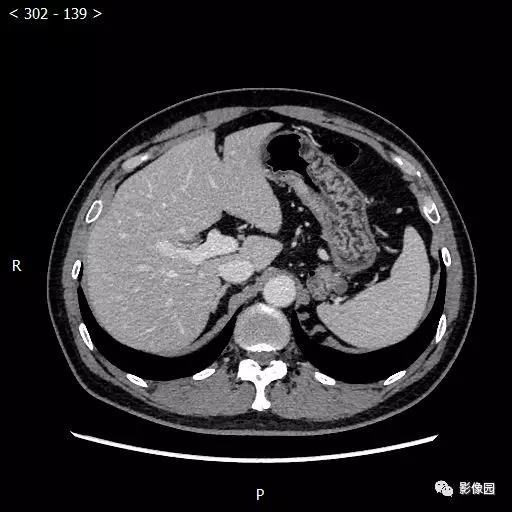
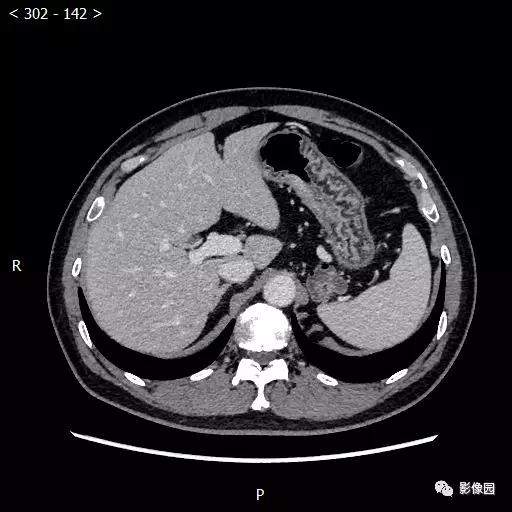
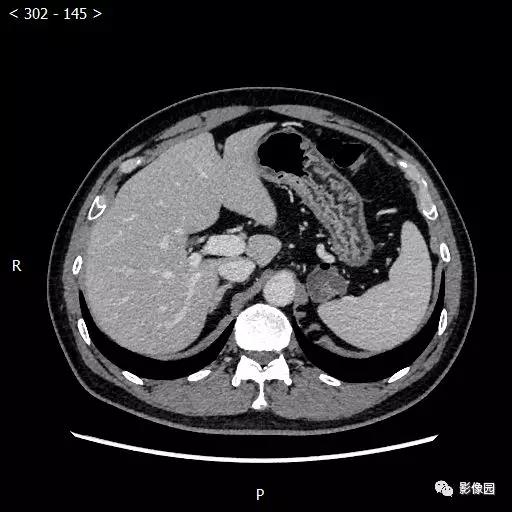
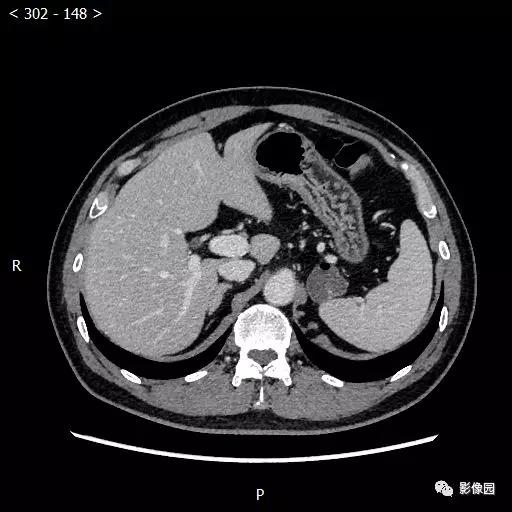
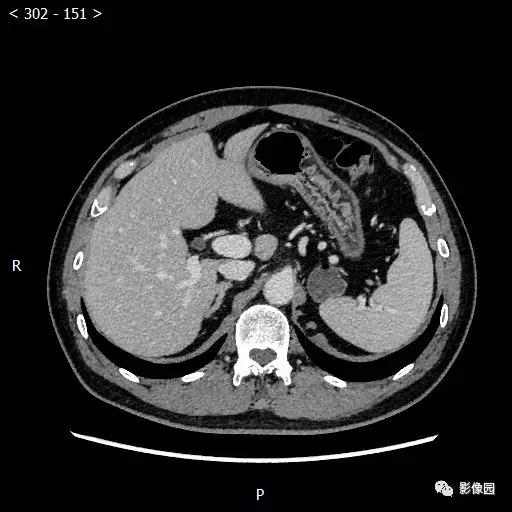
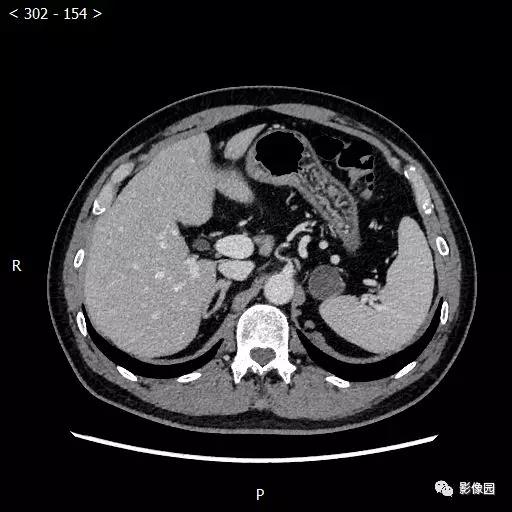
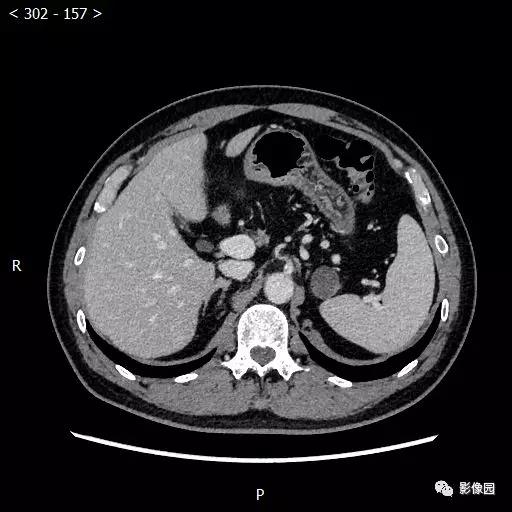
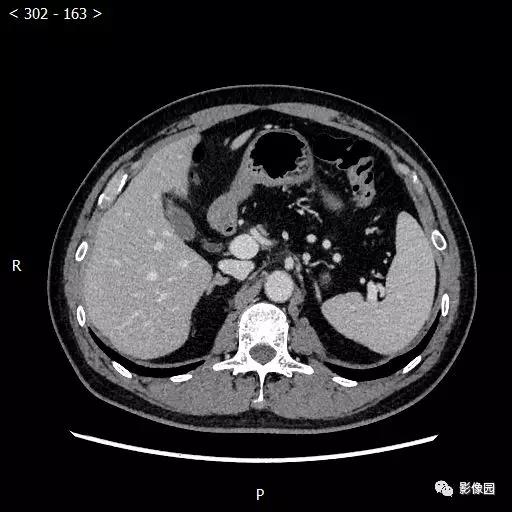
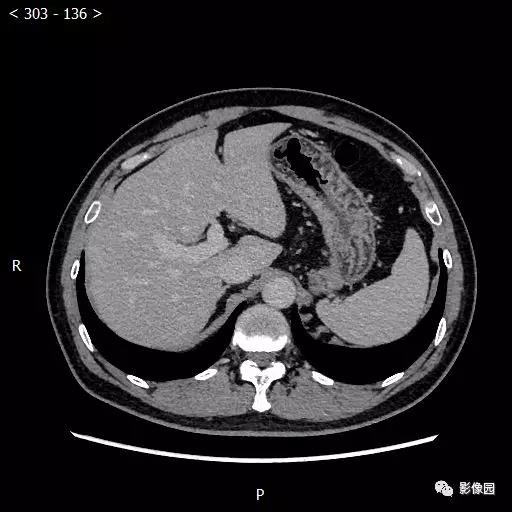
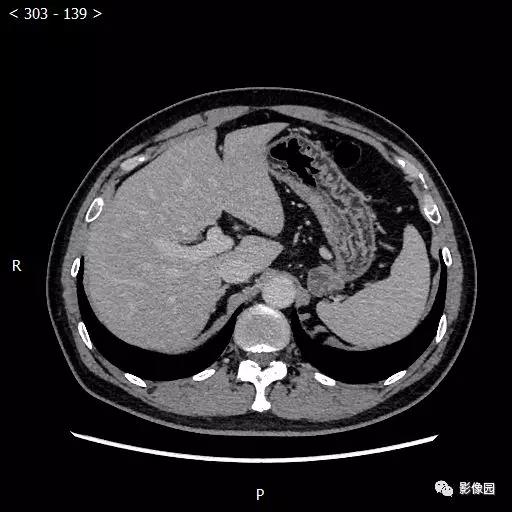
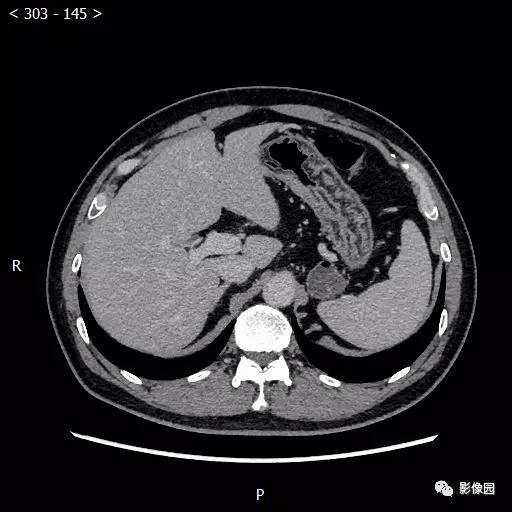
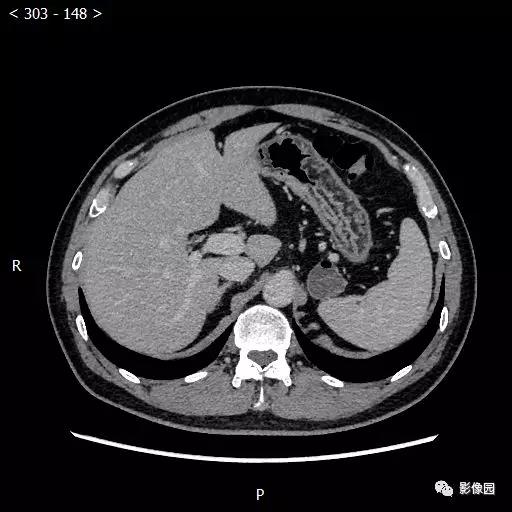
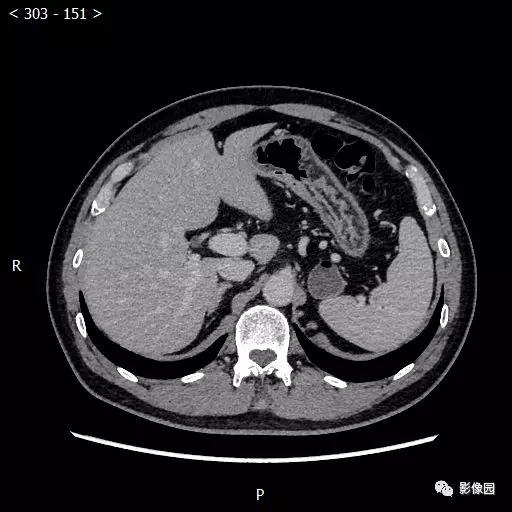
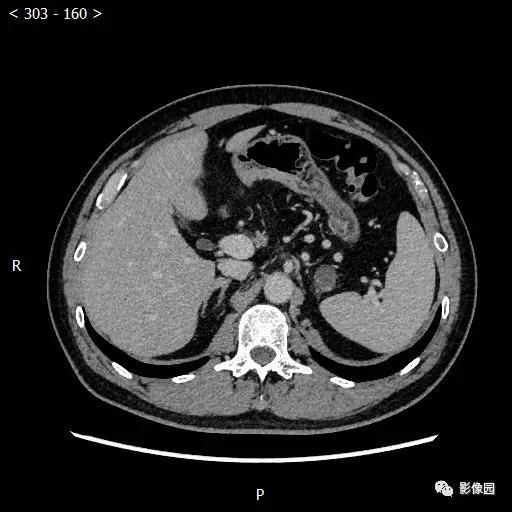
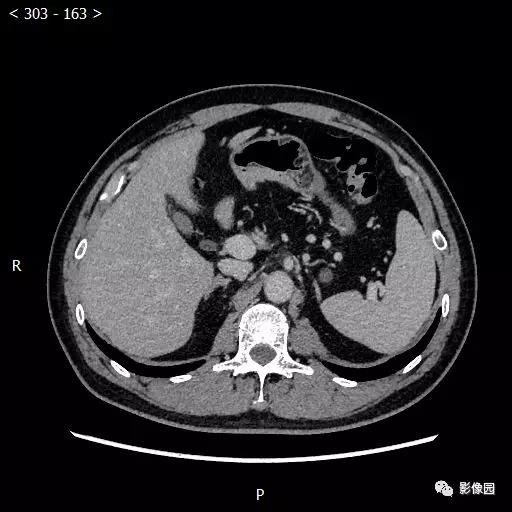
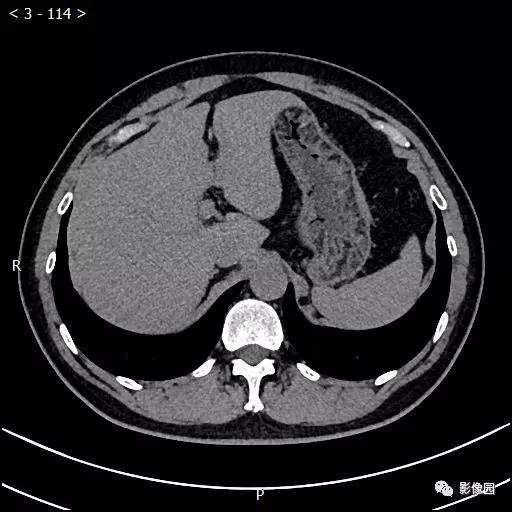
老年男性,间断腹痛10余年,请诊断!
2019-08-06 不详 影像园
患者10余年前出现间断腹痛,位于剑突下,程度较轻,为持续性隐痛,不伴放射,进食后疼痛可能缓解,持续数十分钟至数小时不等。患者无反酸、嗳气,无恶心、呕吐,无腹胀、腹泻。曾于外院行胃镜检查示“浅表性胃炎”,位于进一步治疗。2个月前开始出现左下腹痛,性质描述不清,程度中等,向左肋下及左腹股沟区放射,伴便意,大便性质正常,排便后腹痛可缓解。











本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













了解一下
107
#老年男性#
71
#间断#
82
了解一下
110
了解一下
114
#腹痛#
72