Front Oncol:伴有肺胸膜侵犯(VPI)的IB期NSCLC (≦3 cm)患者的手术治疗模式和预后
2022-02-23 yd2015 MedSci原创
研究表明,对于伴有VPI的IB期NSCLC (≦3 cm)患者,肺叶切除术优于楔形切除术,与肺段切除术类似,而辅助化疗不能使这些患者受益。
近期,四川大学华西医院团队在Frontiers in Oncology杂志上发表了一项研究成果,主要是在早期小肿瘤非小细胞肺癌(NSCLC)伴有肺胸膜侵犯(VPI)患者中,比较肺叶切除、肺段切除和楔形切除的生存率差异,以及辅助化疗的作用。
研究纳入SEER数据库中2004-2015年期间诊断为外周型NSCLC,伴有VPI且大小≦3cm的患者。我们采用多变量分析的Cox比例风险模型,通过倾向得分匹配法(PSM)和Cox回归法进行亚组分析,找出对这些患者的最佳治疗方案。
共有1993例患者纳入研究,中位年龄为70岁(范围为35 ~ 96岁),其中80例(4.0%)接受了放疗。所有患者均行手术,其中肺叶切除术1420例(71.2%),节段切除术116例(5.8%),楔形切除术457例(22.9%)。在主要研究队列中,中位随访时间为33个月(范围为1-83个月)。1年、3年和5年总生存率分别为92.8%、73.9%和60.8%。按手术入路划分,肺叶切除术、节段切除术和楔形切除术的5年OS率分别为66.0%、51.8%和46.7%。然后,我们从初步研究队列中剔除了接受过放疗的患者,形成了确切的研究人群,并进行了生存分析。
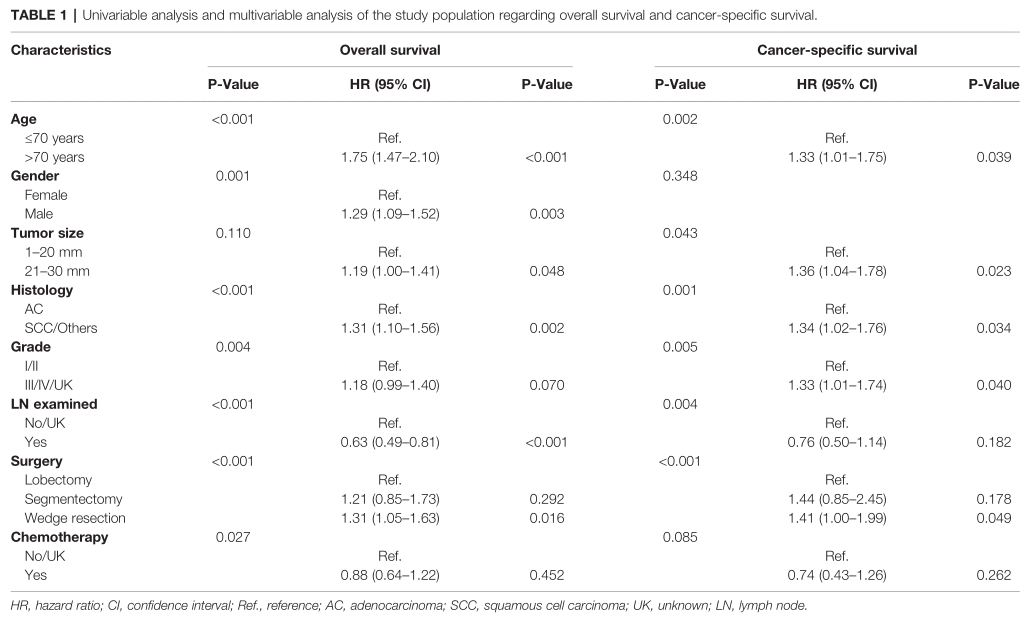
在多变量分析中,年龄、性别、组织学、病理分级、淋巴结检查和手术入路是影响OS的独立预后因素。年龄超过70岁(HR = 1.75;95%CI,1.47-2.10;P<0.001),男性(HR = 1.29;95%CI,1.09-1.52;P = 0.003)、21-30 mm (HR = 1.19;95%CI,1.00-1.41;P = 0.048)、鳞状细胞癌或其他组织学类型(HR = 1.31;95%CI, 1.10-1.56;P = 0.002),接受楔形切除(HR = 1.31;95%CI1.05-1.63;P = 0.017)与较差的OS相关。
通过PSM法比较肺叶切除术和亚叶切除术的OS差异,发现肺叶切除术的OS更好(HR = 1.41;95%CI, 1.08 -1.83;P = 0.011)。在三种手术方式的生存差异比较中,只有楔形切除术明显劣效于肺叶切除术(HR = 1.64;95%CI: 1.22-2.20),其余无统计学差异(肺段切除术与肺叶切除术,P = 0.735;楔形切除术与肺段切除术,P = 0.746)。
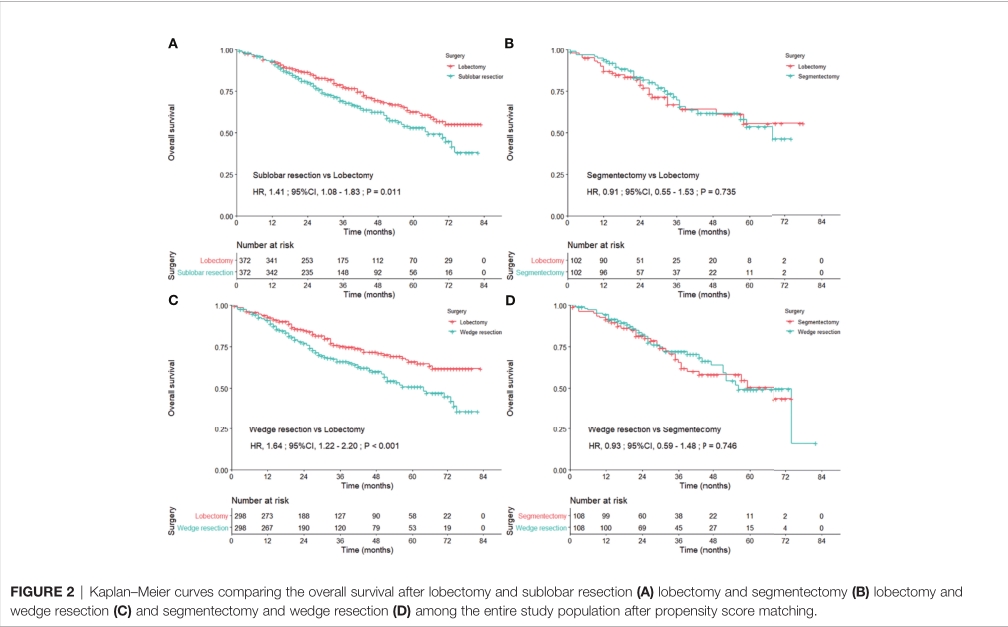
在年龄小于70岁的患者中,接受肺叶切除术的患者OS显著优于接受亚叶切除术的患者(HR = 1.81;95% CI, 1.13-2.90),同样在女性(HR = 1.75;95% CI, 1.21-2.53),大小为1-20mm (HR = 1.61;95%CI,1.11-2.33)患者中。

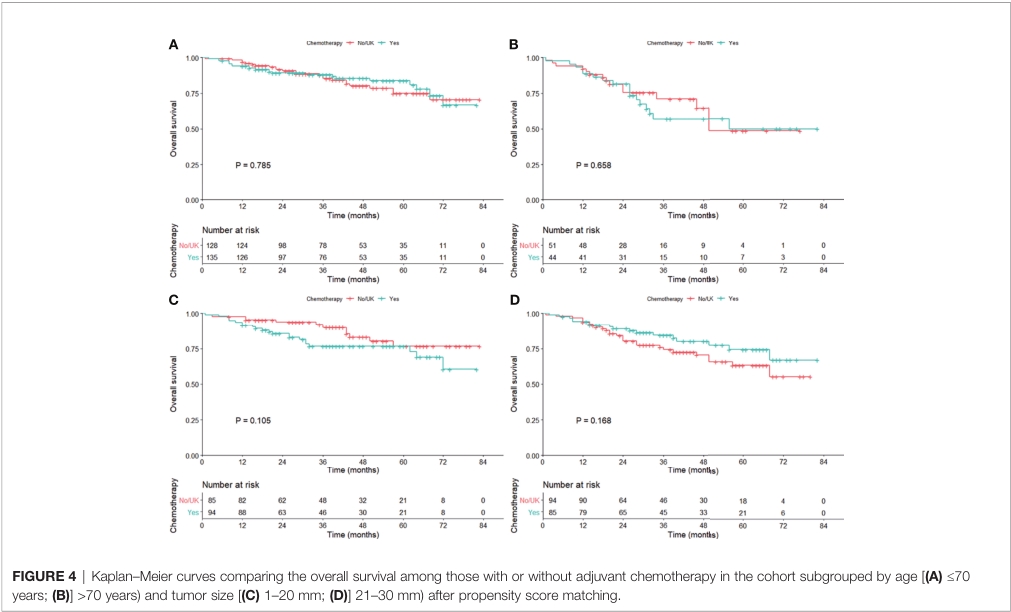
使用辅助化疗未观察到生存获益,亚组分析亦如此。按肿瘤大小分层时,未观察到统计学差异(1-20mm, P = 0.105;21-30 mm, P = 0.168)。
综上,研究表明,对于伴有VPI的IB期NSCLC (≦3 cm)患者,肺叶切除术优于楔形切除术,与肺段切除术类似,而辅助化疗不能使这些患者受益。
原始出处:
Huang W, Deng H-Y, Lin M-Y, Xu K, Zhang Y-X, Yuan C and Zhou Q (2022) Treatment Modality for Stage IB Peripheral Non-Small Cell Lung Cancer With Visceral Pleural Invasion and ≤3 cm in Size. Front. Oncol. 12:830470.doi: 10.3389/fonc.2022.830470.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Ib期#
49
#Oncol#
57
#胸膜#
68
#手术治疗#
76
#治疗模式#
0