Science Advances:巴西研究:遗传变异会增加患癌症的风险
2020-06-30 转化医学网 转化医学网
遗传变异是指生命在遗传的基础上,同一基因库中不同个体之间在DNA水平上的差异,也称“分子变异(molecular variation)”,是对同一物种个体之间遗传差别的定性或定量描述。遗传与变异,是生
变异在生物体上泛指生物种与个体之间的各种差异,包括形态、生理、生化以及行为、习性等各方面的歧异,变异是生物进化和人类育种的根源,包括可遗传的和不可遗传的变异。
由于环境影响和基因型之间相互作用,表现为种群的个体表型变异、环境变异、遗传变异,这是生物进化的一个主要因素。
圣犹达儿童研究医院(St. Jude Children’s Research Hospital)的科学家们与全球合作伙伴正在共同研究巴西后裔中发现的一种常见的TP53-R337H变体。研究人员发现,当肿瘤抑制基因XAF1的一个变体与遗传TP53-R337H突变结合会增加患癌的风险。这项研究结果在6月24日在线发表在《科学进展》(Science Advances)杂志上。
圣犹达病理学博士、该研究的通讯作者艾米莉亚·平托(Emilia Pinto)表示,“我们期待这些结果对公众健康有重大影响。一旦临床医生知道要寻找什么样的变体,他们就能更好的管理那些更高癌症风险的患者。
一项20年来的发现
20多年前,以劳尔·里贝罗(Raul Ribeiro)博士领导的圣犹达大学研究人员在巴西人中发现了TP53-R337H遗传变异。平托和她的同事随后发现TP53-R337H是一种创生突变,是在巴西殖民时期引入的。TP53-R337H在一般人群中很少见,但在巴西很常见。每300个巴西人中就有一个是这样。
圣犹达病理学的教授、该论文的资深作者拉杰德·赞比蒂(Gerard Zambetti)表示,“TP53-R337H突变不能解释全部的癌症风险。携带TP53-R337H基因的个体之间的差异可能导致一些人患上多种癌症,一些人患上一种癌症,还有一些人根本不会患上癌症。”
在全基因组测序研究中,研究人员在TP53-R337H突变载体的一个子集中发现了肿瘤抑制基因XAF1的变异。遗传了XAF1突变和TP53-R337H突变的个体比那些仅遗传TP53-R337H突变的个体患癌症的风险更大。
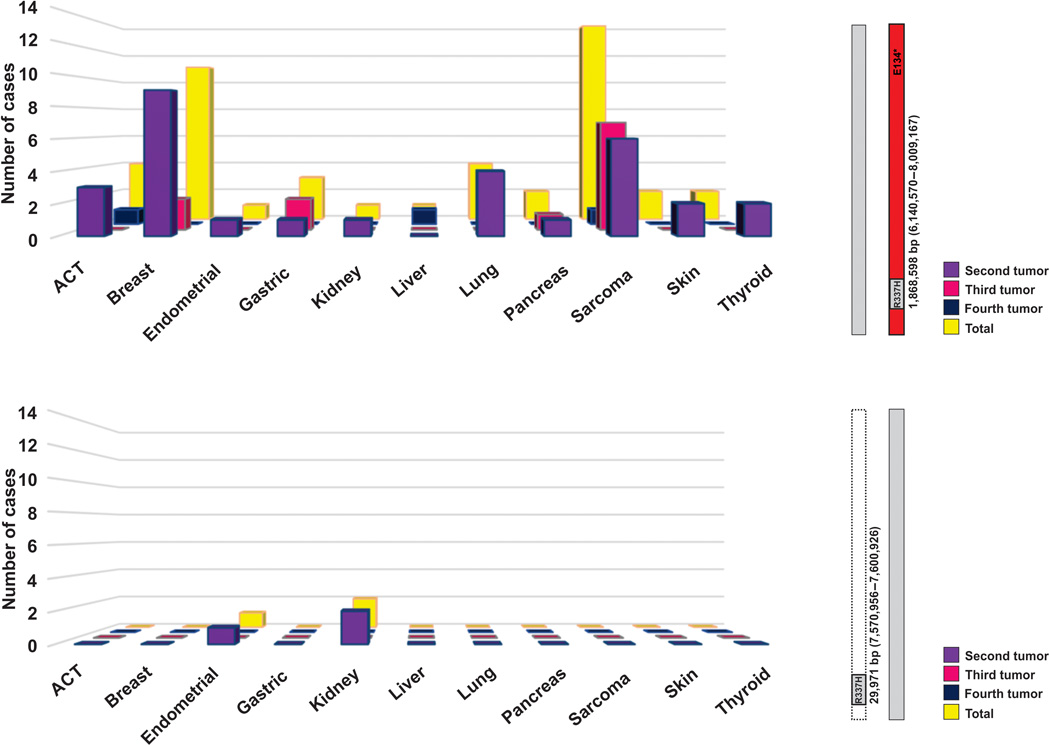
在只有R337H和扩展单倍型的患者中,肿瘤类型作为第二、第三或第四种恶性肿瘤的分布。
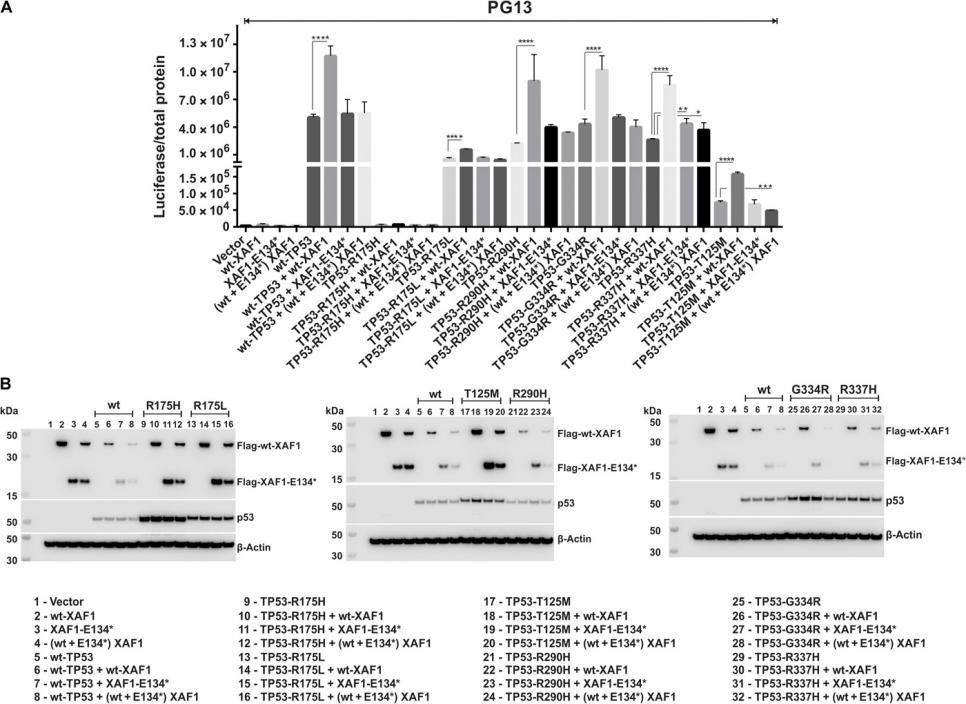
XAF1增加了TP53亚型的转录活性。
TP53突变在罕见的小儿肾上腺皮质癌患者中很常见。然而,TP53突变是许多其他类型癌症的一个重要因素。对XAF1修饰TP53Dev认识,可能会推动进一步的研究这个靶点能否成为新的治疗策略的基础。
这一发现有助于调整公共卫生方法
圣犹达大学的研究人员通过对巴西血统的个体进行全基因组测序,研究了这种变异的原因。通过圣犹达环球建立的伙伴关系是获得开展这项工作所需样本的关键。
在全球儿科医学部的领导下,圣犹达环球公司成立了圣犹大全球联盟(St. Jude Global Alliance),包括亚太地区、中美洲和南美洲、中国、东部和地中海地区、欧亚大陆、墨西哥和撒哈拉以南非洲地区的项目。
如果没有世界各地的伙伴的合作,这项研究是不可能完成的。这些结果将对巴西的公共卫生产生影响,对整个儿科癌症团体很重要。”
原始出处:
Emilia M. Pinto, et al. XAF1 as a modifier of p53 function and cancer susceptibility. Science Advances 24 Jun 2020: Vol. 6, no. 26, eaba3231. DOI: 10.1126/sciadv.aba3231.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#变异#
53
#SCIE#
52
#遗传变异#
68
#巴西#
53
#患癌#
59