FDA允许开展Silmitasertib治疗COVID-19患者的II期临床试验
2020-11-07 Allan MedSci原创
生物制药公司Senhwa Biosciences今日宣布,已收到美国食品和药品监督管理局(FDA)肯定回复,将开始II期临床试验,以评估Silmitasertib治疗中度COVID-19患者的有效性。
生物制药公司Senhwa Biosciences今日宣布,已收到美国食品和药品监督管理局(FDA)肯定回复,将开始II期临床试验,以评估Silmitasertib治疗中度COVID-19患者的有效性。该II期试验是一项单中心、开放标签、随机对照的干预性前瞻性研究,预计将招募20名中度COVID-19患者。

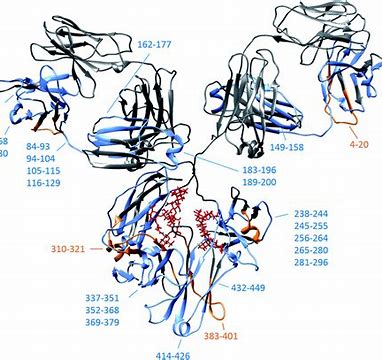
Silmitasertib是一种口服型酪蛋白激酶2(casein kinase2,CK2)抑制剂,它预计能够阻止病毒(SARS-CoV-2)快速复制并阻止传播到附近健康细胞,又能够抑制不受控制的炎症反应。CK2是一种高度保守的、在各种真核生物中都广泛存在,并且具有多种生理功能的磷酸化丝氨酸/苏氨酸的激酶。CK2全酶是由两个α催化亚基和两个β调节亚基构成的异源四聚体,但CK2单体也可以独立发挥一定的生理功能。
Senhwa Biosciences首席医学官John Soong博士说:“FDA此项批准了对于Silmitasertib而言是一个重要的里程碑,这代表了治疗病毒性疾病免疫反应失调的新范例”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#I期临床#
60
#I期临床试验#
61
#II期临床试验#
72
#MIT#
70
#COVID-19患者#
69
#II期临床#
62