Cell Metab:魏海明/田志刚合作组揭示NK细胞丧失抗肿瘤功能背后的代谢调控过程
2018-07-20 BioArt BioArt
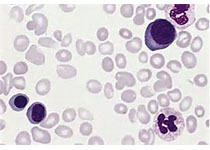
自然杀伤细胞 (natural killer cell,NK细胞) 是一种效应淋巴细胞,在机体抵抗肿瘤过程中发挥至关重要的作用。NK细胞无需预先致敏,即能够直接杀伤肿瘤细胞,并且能够通过分泌细胞因子促进适应性免疫的抗肿瘤作用。基于上述原理,NK细胞在肿瘤免疫治疗中的价值已得到广泛认可。然而,越来越多的研究表明,肿瘤生长过程中,肿瘤细胞可以通过多种机制诱导NK细胞功能紊乱,从而逃避NK细胞的监视,这
近几年来,代谢调控在肿瘤、免疫、表观遗传等领域越来越受重视,对于NK细胞来说相关的代谢研究较少,目前主要集中在糖代谢调控与NK细胞功能方面。然而糖代谢的变化与NK细胞在肿瘤中的效应功能相关的而研究目前并不清楚。
2018年7月19日,Cell Metabolism在线发表了中国科学技术大学生命科学与医学部、中科院天然免疫与慢性疾病重点实验室和合肥微尺度物质科学国家研究中心魏海明教授和田志刚教授课题组合作研究的论文Dysfunction of Natural Killer Cells by FBP1-induced Inhibition of Glycolysis during Lung Cancer Progression,该项研究成果展示了肿瘤发生发展过程中自然杀伤细胞(NK细胞)的动态改变,并从糖代谢调控的角度揭示了一种NK细胞功能紊乱的新机制。
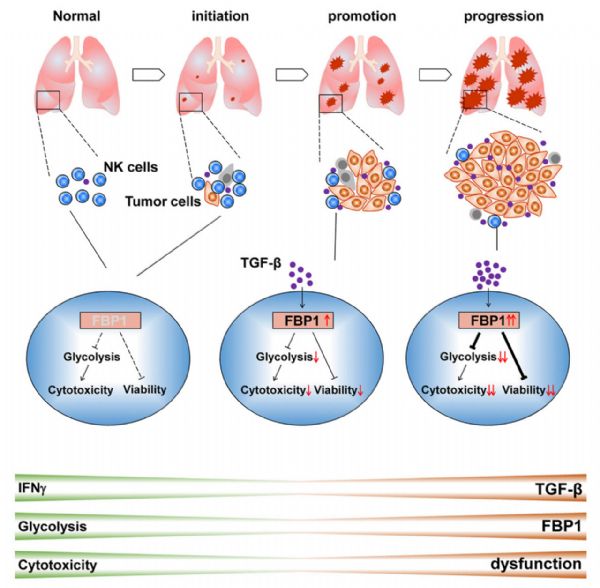
在这项研究中,研究人员利用Kras突变自发肺癌小鼠模型。研究表明,在肿瘤起始期,NK细胞有强大的抗肿瘤功能,但是在肿瘤促进期和进展期,NK细胞丧失了抗肿瘤能力。进一步研究发现,NK细胞丢失抗肿瘤能力与其自身功能紊乱密切相关,当肺癌发生后,肿瘤微环境累积大量TGF-β,进而促进NK细胞上调表达果糖-1,6-二磷酸酶 (Fructose 1,6-bisphosphatase,FBP1) 基因(FBP1是糖异生途径中的关键酶,该酶缺陷导致糖异生障碍,致使上游底物堆积和低血糖)。异常表达的FBP1抑制细胞自身糖酵解代谢,同时破坏细胞存活能力,最终导致NK细胞功能紊乱。而抑制NK细胞的FBP1活性,能够恢复NK细胞效应功能、存活能力和体内杀瘤能力。
总的来说,该研究通过小鼠肺癌模型,发现在肿瘤生发展过程中NK细胞是如何受肿瘤微环境的影响通过糖代谢调控逐步功能紊乱最终丧失其强大的抗肿瘤功能(FBP1能够通过抑制NK细胞糖酵解代谢从而削弱NK细胞功能)。这从一定程度上丰富了人们对NK细胞在与肿瘤细胞相互较量过程的认识,而靶向FBP1提高NK细胞功能可以作为优化NK细胞肿瘤免疫治疗的新策略。
据悉,第一作者为中国科大丛靖婧博士,魏海明教授和田志刚教授为论文共同通讯作者。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#MET#
81
#Meta#
82
#CEL#
78
#Cell#
80
一起学习学习
98