2018AHA/ACC胆固醇临床实践指南更新:新指南,新在哪?
2018-11-13 中国心血管健康联盟进阶学院 MedSci原创
美国中部时间2018年11月10日,2018美国心脏协会(AHA)科学年会在美国芝加哥盛大开幕。会议伊始,即公布了新版AHA/ACC胆固醇临床实践指南。旧版指南更新于2013年,距今已有五年时间,在此期间非他汀类药物依折麦布与PCSK9抑制剂相继上市,又有多项重要研究问世,新版指南究竟会作何推荐?
美国中部时间2018年11月10日,2018美国心脏协会(AHA)科学年会在美国芝加哥盛大开幕。会议伊始,即公布了新版AHA/ACC胆固醇临床实践指南。旧版指南更新于2013年,距今已有五年时间,在此期间非他汀类药物依折麦布与PCSK9抑制剂相继上市,又有多项重要研究问世,新版指南究竟会作何推荐?
新版胆固醇指南十大要点精炼
Scott Grundy教授作为指南撰写小组主席,率先对指南更新的十大要点进行解读!
1. 所有人在整个生命期间均应保持有益心脏健康的生活方式
2. 对于临床ASCVD患者,采用高强度或最大耐受剂量的他汀治疗以降低LDL-C水平。
· 通过他汀降低更多的LDL-C,随之风险也就越低。采用最大耐受剂量的他汀可降低50%以上的LDL-C水平。
3. 对于极高风险的ASCVD患者,如果LDL-C水平不能达到70mg/dL(1.8mmol/L),应考虑在他汀药物的基础上使用非他汀类降脂药。
· 极高风险包括发生多种严重ASCVD事件或1次严重ASCVD事件伴多种危险情况
· 对于极高风险的ASCVD患者如果最大耐受剂量的他汀不能将LDL-C降至70mg/dL(1.8mmol/L)以下,可依次添加依折麦布和PCSK9抑制剂。
4. 严重原发性高胆固醇血症患者(LDL-C水平≥190mg/dL),可不计算10年ASCVD风险,直接应用高强度他汀治疗。
· 如果LDL-C水平仍然≥100 mg/dL(≥2.6 mmol/L),可联合依折麦布进行治疗。
· 如果他汀联合依折麦布后LDL-C水平仍然≥100 mg/dL(≥2.6 mmol/L)且有多种ASCVC风险增高危险因素的患者,可考虑使用PCSK9抑制剂,尽管其长期安全性(>3年)仍不确定。
5. 对于40-75岁糖尿病且LDL-C≥70 mg/dL(≥1.8 mmol/L)的患者,可不计算10年ASCVD风险,直接应用中等强度他汀类治疗。
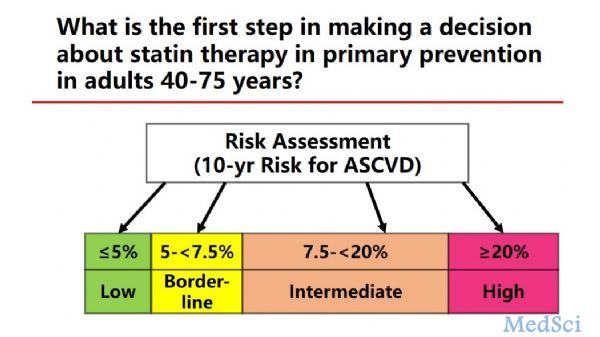
6. 对于40~75岁需要ASCVD一级预防的成人,应在使用他汀前,与患者讨论风险。
7. 对于40~75岁无糖尿病且LDL-C水平≥70 mg/dL(≥1.8 mmol/L)的成年人,如
·10年ASCVD风险≥7.5%,在讨论后倾向于他汀治疗可应用中等强度他汀治疗。
·如无法确认风险水平,可采用冠状动脉钙化(CAC)进行判断。
8. 对于40-75岁无糖尿病但10年风险在7.5%-19.9%(中危)患者,如果存在风险加强因素,可开始他汀治疗。
9. 对于40-75岁无糖尿病但10年风险在7.5%-19.9%患者,如果无法确定他汀治疗剂量,可考虑检查CAC。
· CAC评分1-99的患者,可采用他汀治疗,特别是年龄55岁以上的患者。
· 如果CAC评分≥100,或≥75th百分位,除非与患者进行风险讨论后有其他方案,否则应采用他汀治疗。
10. 启动他汀或剂量调整后4~12周后应复查血脂,观察LDL-C百分比降幅以及对生活方式改变和药物治疗的依从性,随后根据需求每3~12月复查一次。
新版指南,更新在哪?
新版指南在2013年指南的基础上,基于5年来最新的循证证据做出修订:
1. 新版指南强调,生活方式改变是预防和治疗ASCVD的基础。
2. 目前,他汀药物仍是ASCVD患者二级预防和ASCVD风险升高患者一级预防的首选药物,指南推荐ASCVD高风险或极高风险的患者应采用高强度或最大耐受剂量的他汀治疗。但同时肯定了他汀联合非他汀类药物治疗的获益。大规模的RCT研究显示在高风险患者中进一步降低LDL-C水平可降低ASCVD风险,虽然新版指南未明确指出及高风险患者的降脂目标,但是对于ASCVD患者和糖尿病患者,若高强度他汀治疗后仍无法将LDL-C水平控制在1.8mmol/L以下,则依次联合依折麦布或PCSK9抑制剂治疗,实际上已经认可了联合降脂方案的疗效和“LDL-C低一些更好”的理论。
3. 新版指南未明确标注各类患者需要降低的胆固醇治疗目标值,强调不同危险分层患者必须降低的LDL-C幅度。ASCVD高风险或极高风险的患者应降LDL-C水平50%以上,中等危险患者LDL-C应降低30%以上。通过他汀治疗后何时启动非他汀药物治疗联合方案(如及高风险ASCVD患者接受高强度他汀治疗后LDL-C水平仍高于1.8mmol/L可联合非他汀类方案)告诉我们理想的LDL-C控制靶标。
血脂管理是ASCVD防治的基石,其研究进展和指南更新对于指导临床降脂治疗和改善ASCVD患者的预后具有重要意义。基于高证据质量的2018AHA/ACC胆固醇临床实践指南发布为临床血脂管理提供了实践指导。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#指南更新#
111
#实践指南#
72
#新指南#
95
学习学习天天学习
103
#AHA#
76
#临床实践#
64
#ACC#
82
#临床实践指南#
61