Chest:危重病患者气管插管体位有讲究!
2017-05-12 xing.T MedSci原创
在这个多中心试验中,倾斜体位并不能改善气管插管期间危重病人的氧合情况,与吸气体位相比。倾斜体位可能会恶化声门Cormack-Lehane分级,增加喉镜插管成功所需的尝试次数。
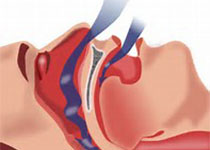
低氧血症是危重病人气管插管最常见的并发症。近日,胸部疾病领域权威杂志Chest杂志上发表了一篇研究文章。研究人员假设在倾斜体位插管可以防止低氧血症,通过增加功能性残气量,减少插管时间,但从来没有在手术室外进行过研究。
研究人员采用在2015年7月22日至2016年7月19日期间4个重症监护病房接受气管内插管的260名成年患者进行了一项多中心、随机试验比较了倾斜体位(床头抬高25度)和吸气体位(躯干仰卧,颈部弯曲,头部延伸)。该研究的主要结果是插管开始到插管结束后两分钟内动脉血氧饱和度的最低值。该研究的次要结果包括声门Cormack-Lehane分级、插管困难和喉镜检查次数。
研究人员发现倾斜体位的中位最低动脉血氧饱和度为93% [IQR为84-99 %],吸气体位为92%[79-98%](P=0.27)。倾斜体位似乎增加III级或IV级的发生率(25.4% vs. 11.5%,P=0.01),增加插管困难的发生率(12.3% vs. 4.6%,P=0.04),并减少第一次尝试插管成功的几率(76.2% vs. 85.4%,P=0.02)。
在这个多中心试验中,倾斜体位并不能改善气管插管期间危重病人的氧合情况,与吸气体位相比。倾斜体位可能会恶化声门Cormack-Lehane分级,增加喉镜插管成功所需的尝试次数。
原始出处:
Matthew W. Semler,et al. A Multicenter, Randomized Trial of Ramped Position versus Sniffing Position during Endotracheal Intubation of Critically Ill Adults.Chest. 2017. http://journal.publications.chestnet.org/article.aspx?articleid=2627076
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Chest#
74
#EST#
62
#危重病#
70
学习了,提高了认识
80
#气管插管#
66
临床研究得很细了
106