Chest :超声技术的应用可使危重病人的胸膜手术更有效更安全
2017-07-23 MedSci MedSci原创
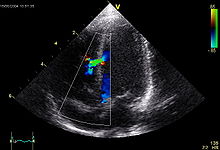
对危重病人来说,从胸膜腔引流液体或空气的手术在技术上是具有挑战性的,而且与严重的并发症有关。与胸腔引流有关的并发症主要有:干抽,膈肌下入针,气胸,相邻结构的损伤以及肋间动脉损伤等。 本文介绍了一种将许多工具纳入常见的临床手术的系统方法,如诊断胸腔穿刺术,治疗引流术,或导管插入。许多技术在演示中包括了一系列的说明性的数字和叙述性的视频介绍。
对危重病人来说,从胸膜腔引流液体或空气的手术在技术上是具有挑战性的,而且与严重的并发症有关。与胸腔引流有关的并发症主要有:干抽,膈肌下入针,气胸,相邻结构的损伤以及肋间动脉损伤等。
本文介绍了一种将许多工具纳入常见的临床手术的系统方法,如诊断胸腔穿刺术,治疗引流术,或导管插入。许多技术在演示中包括了一系列的说明性的数字和叙述性的视频介绍。本文中提出的建议是作者的观点,虽然它们代表了解决常见问题的合理方法,但值得注意的是,也有许多可替代方法和同样合理的方法可能受到其他提供者的青睐。
可将这种胸腔引流手术的整体方法分为9个单独的技术:
技术1:定位隔膜
技术2:估计积液的大小
技术3:定位肋间动脉
技术4:测量最小和最大距离
技术5:进行超声辅助胸腔引流
技术6:进行超声引导的胸膜腔引流
技术7:在膨胀前检查导丝的位置
技巧8:排除术后的气胸
技术9:在抽气胸时使用超声波技术
原始出处:
Scott J. Millington, Seth Koenig. Better with Ultrasound: Pleural Procedures in Critically Ill Patients. Chest. 2017 July.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#EST#
61
#胸膜#
75
#危重病#
76
#Chest#
62
#超声技术#
80
#危重病人#
76