孤立性肺栓塞(PE)患者与深静脉血栓形成(DVT)相关性肺栓塞患者具有明显不同的临床特征,伴有更多的肺部疾病和动脉粥样硬化。这些发现表明,在孤立性肺栓塞中可能存在独特的分子病理生理特征和不同的参与信号通路。
为了验证上述推测,研究人员分析了一项多中心的前瞻性队列研究“静脉血栓栓塞的基因型和分子表型[GMP-VTE]项目”的532位受试者的数据。
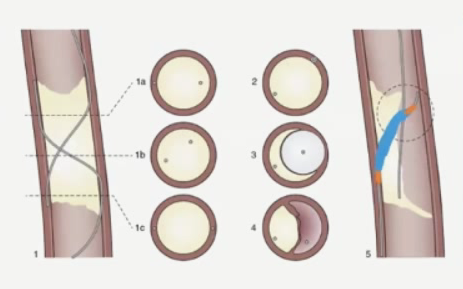
这532位受试者,包括96位孤立性肺栓塞患者、276位DVE相关性肺栓塞患者和160位孤立性DVT患者。研究人员采用靶向高通量蛋白质组学、机器学习和生物信息方法对比了不同疾病患者急性期的血浆蛋白质组。
经过对比分析发现,不同表型的肺栓塞之间存在相同的分子过程,同时也鉴定出了孤立性肺栓塞所特有的蛋白标记。共有的过程包括炎症上调、对氧化应激应答以及肺表面活性物质丧失。孤立性肺栓塞所特有的蛋白标记包含5种蛋白:干扰素-γ (IFNG)、胶质细胞源性神经营养生长因子(GDNF)、多肽N-乙酰半乳糖胺基转移酶3 (GALNT3)、2型肽基精氨酸脱亚氨酶 (PADI2) 和白介素-15受体α亚基(IL-15Rα)。使用顺式蛋白质定量性状位点(cis pQTL)对这些蛋白进行了正交验证。
在一个独立的以人群为基础的队列(n=5,778)中进行了外部验证,进一步验证了上述蛋白质组学结果,还发现这些蛋白可预测无VTE病史的个体发生原发性孤立肺栓塞的可能性(中位发生时间:2.9年,四分位范围:1.6-4.2年),提示这些蛋白可能参与孤立性肺栓塞的早期发病机制。
简而言之,该研究鉴定出了不同VTE表型之间的相似的以及不同的分子病理。特别是,在孤立性PE的急性病理生理过程中,介导VTE发生的非典型通路更常于合并呼吸道和动脉粥样硬化疾病的患者中发挥作用。
原始出处:
Vincent Ten Cate, et al. Protein expression profiling suggests relevance of non-canonical pathways in isolated pulmonary embolism. Blood. February 02, 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Blood#点击进入话题查看更多相关文章 或评论时插入话题加入讨论
123
#孤立性#
118
涨知识
110
开拓了视野
121