Hypertension:血清镁与高血压和慢性肾脏疾病进展风险的关系
2021-11-05 MedSci原创 MedSci原创
在CKD患者中,较高的血清镁与较低的SBP和DBP以及较低的高血压和CKD进展风险相关。在CKD患者中,补充镁是否可以优化血压控制并防止疾病进展值得进一步研究。
慢性肾病 (CKD) 是众所周知的公共卫生问题,在美国影响约3400万成年人,占美国人口的14%以上。有研究报道镁离子参与了血压(BP)调节。血清镁异常在慢性肾脏病(CKD)患者中很常见,但其与CKD患者高血压和CKD进展之间的关联尚未明确。

近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员分析了来自慢性肾功能不全队列(CRIC研究)的3866名参与者的数据。线性回归评估了血清镁与基线收缩压(SBP)和舒张压(DBP)之间的关联。研究人员采用Logistic回归探讨了血清镁与各种高血压之间的关联,并采用Cox比例风险模型评估了高血压与CKD进展风险的关系。
受试者平均血清镁水平为2.0mEq/L(±0.3mEq/L)。较高的镁水平与较低的SBP(-3.4mmHg[95%CI为-5.8至-1.0每1mEq/L])和较低的DBP(-2.9mmHg[95%CI为-4.3至-1.5每1mEq/L])相关。较高的镁水平与基线时根据美国心脏协会定义的高血压(SBP≥130mmHg或DBP≥80mmHg)较低风险相关(调整后的风险比为0.65[95%CI为0.49-0.86/1mEq/L]),以及与较低的血压控制不佳风险(SBP≥120mmHg或DBP≥80mmHg;调整后的比值比为0.58[95%CI为0.43-0.78每1mEq/L])相关。
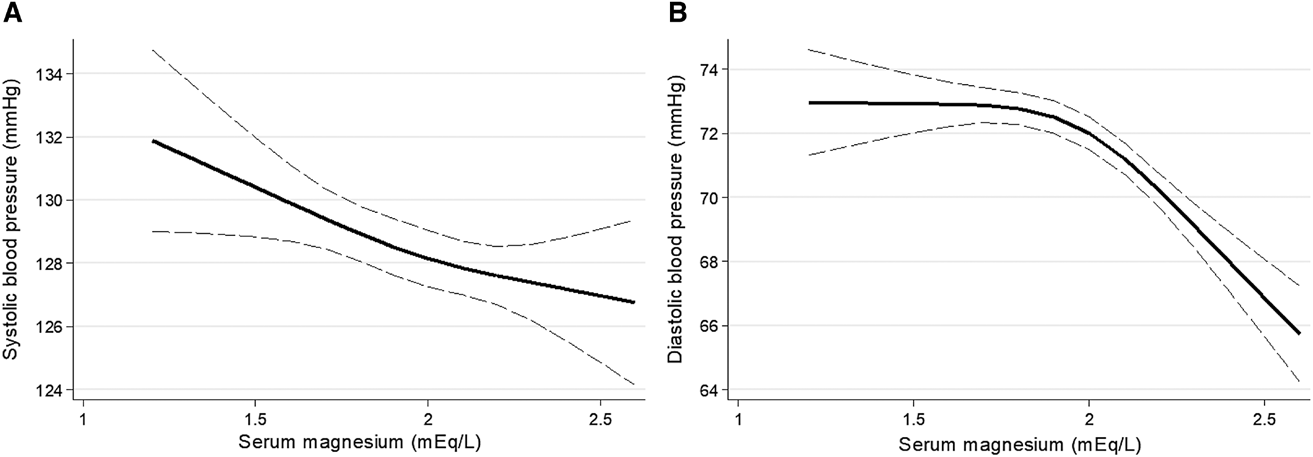
在事件时间分析中,较高的基线血清镁与较低的根据CRIC定义的高血压事件风险相关(调整后的风险比为0.77[95%CI为0.46-1.31/1mEq/L])。较高的镁水平与CKD进展的风险显著降低相关(调整后的风险比为0.68[95%CI为0.54-0.86每1mEq/L])。
由此可见,在CKD患者中,较高的血清镁与较低的SBP和DBP以及较低的高血压和CKD进展风险相关。在CKD患者中,补充镁是否可以优化血压控制并防止疾病进展值得进一步研究。
原始出处:
Simon Correa.et al.Serum Magnesium, Blood Pressure, and Risk of Hypertension and Chronic Kidney Disease Progression in the CRIC Study.Hypertension.2021.https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.121.17694
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
55
#疾病进展#
102
#风险的关系#
65
#TENS#
70
#Hypertension#
59
#慢性肾脏#
99
好!
83