Cell:同病不同药?单细胞图谱揭示溃疡性结肠炎的耐药机制
2019-07-30 苏煜静 生物探索
近日,据爱尔兰邮报报道:爱尔兰瑞安航空公司引发了人们的议论,原因是拒绝为26岁患有溃疡性结肠炎的女孩Alicia Dillon免费提供靠近洗手间旁的座位。瑞安航空给出的理由是他们承诺满足有额外需求的残疾人,但Dillon并不在列。
近日,据爱尔兰邮报报道:爱尔兰瑞安航空公司引发了人们的议论,原因是拒绝为26岁患有溃疡性结肠炎的女孩Alicia Dillon免费提供靠近洗手间旁的座位。瑞安航空给出的理由是他们承诺满足有额外需求的残疾人,但Dillon并不在列。
爱尔兰邮报官网截图
对于不了解溃疡性结肠炎的人很难想象Dillon的痛苦。溃疡性结肠炎(UC)是一种慢性、进展性、炎症性肠道疾病。UC患者往往腹痛难忍,伴随持续性腹泻,甚至会出现直肠出血和体重减轻等症状。在美国大约有90.7万UC患者,整个欧洲大约有100万UC患者。然而目前我们还不清楚溃疡性结肠炎背后的发病机制。即便是有相同诊断的UC病患也可能对治疗产生截然不同的反应。
近日,麻省理工学院和哈佛大学的研究学者通过溃疡性结肠炎的高清单细胞图谱探究了肠道组织成分变化和不同细胞类型之间相互作用是如何影响疾病的,并且确定了与疾病相关的细胞和通路基因在这其中扮演的角色。这份单细胞图谱为提高UC患者诊断治疗水平奠定了坚实基础。该研究结果发表在《Cell》杂志上。
该研究的第一作者Christopher Smillie,Moshe Biton和JoséOrdovas-Monta?es为了了解细胞类型特异性和作用途径,从18例UC患者和12例健康人的结肠粘膜中生成了366,650个细胞的图谱,揭示了51个上皮细胞、基质细胞和免疫细胞亚群。
多种细胞群共同作用
研究对比了UC患者与健康个体的组织样本,结果显示许多UC风险基因是具有细胞类型特异性的,并且受到相对较少的基因调控通路的共同调控。 这表明某些细胞的比例及它们之间可能的相互作用存在显着的差异。像是在UC患者样本中,与炎症相关的一种特殊类型的成纤维细胞以及同时表达CD8和IL-17的T细胞所占比例更高。
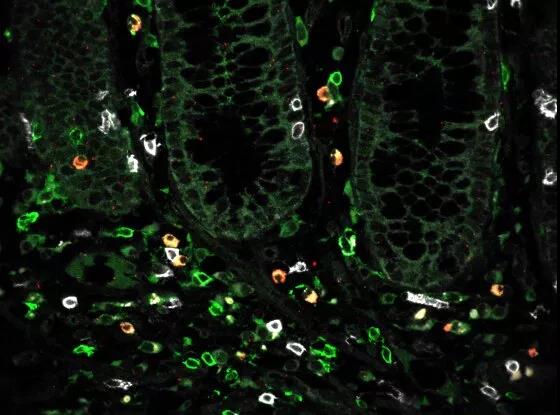
在发炎的结肠组织中表达CD4(绿色),CD8(白色)和IL-17(红色)的T细胞的快照
此外,研究小组还发现了一种名为微纤维细胞(microfold-like cells)的上皮细胞的罕见细胞亚群。这种细胞通常只出现在小肠中,但在UC患者的结肠中同样也发现了该细胞。
研究人员发现,多种细胞群相互发送信号,并控制不同细胞亚群之间的其他相互作用。这表明病变结肠中的细胞网络发生了重大重组。
溃疡性结肠炎的耐药性有了新解释
研究数据表明,新的细胞亚群可能与耐药性有关,而耐药性影响着约三分之一的患者,这些细胞亚群或可能与增加溃疡性结肠炎风险的其他基因有关。继而,研究人员进一步深入了解溃疡性结肠炎患者耐药的可能机制。
在UC患者中,肿瘤坏死因子(TNF)蛋白水平较高,抗TNF药物可减轻炎症并治愈许多患者的组织。然而,大约30%的患者对治疗没有响应,而那些有响应的患者随着时间的推移变得具有耐药性。
研究人员此前已经确定了耐药性相关的基因,但尚不清楚结肠中哪些特定的细胞类型表达了这些基因。
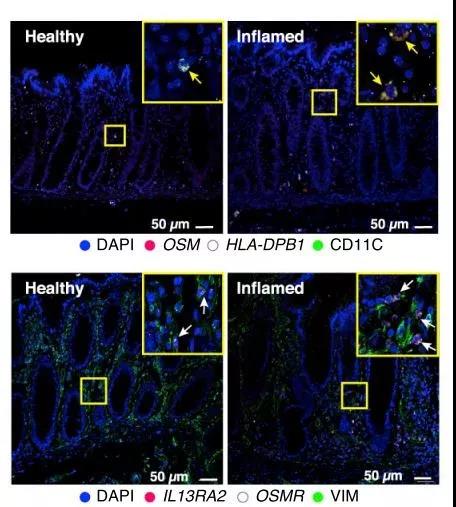
IAFs和单核细胞通过OSM信号通路与抗tnf耐药相关
在此次研究中, 单细胞数据分析结果表明,产生耐药性的罪魁祸首之一是与炎症相关的成纤维细胞。这项研究明确了成纤维细胞可能与其他细胞相互作用以促进耐药性,并诱发成纤维细胞对一种名为OSM的信号分子作出反应,从而绕过TNF通路产生耐药性。
将来有一天,这一发现可能被用来帮助识别可能产生耐药性的患者。有这些耐药性标志物的患者可以提前诊断。或许还可以针对这些特定细胞,结合与抗TNF治疗相关的药物来治疗。
人类细胞基因图谱再创佳绩
这项研究是国际人类细胞图谱项目的一部分。以前对溃疡性结肠炎患者的基因研究发现了基因组中许多与疾病相关的区域,但研究人员往往不知道这些基因在哪些细胞和通路中发挥作用,这阻碍了他们的进一步研究。
新的细胞图谱帮助研究者确定表达这些基因的细胞类型及其可能的功能。这份细胞图谱还为确定哪些细胞亚群在其他疾病中表达相关的遗传变异提供了一个通用指南。
原始出处:Christopher S. Smillie, Moshe Biton, Jose Ordovas-Montanes, et al. Intra- and Inter-cellular Rewiring of the Human Colon during Ulcerative Colitis. Cell. JULY 25, 2019
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#单细胞图谱#
80
#溃疡性#
0
#Cell#
52
#细胞图谱#
65
#耐药机制#
73
#CEL#
53
学习了
103
是一种指纹图谱吧?
85
谢谢了,学习
90