ERJ:CILP1 作为肺动脉高压引起的右心室适应不良的生物标志物
2021-10-11 刘少飞 MedSci原创
肺动脉高压 (PH) 导致右心室 (RV) 压力超负荷,这最初会导致适应性 RV 变化,例如壁厚和收缩性增加。然而,持续增加的后负荷会导致适应不良的病理重构、心室动脉解偶联和右心衰竭。

 众所周知,右心衰竭(RV)是肺动脉高压(PAH)死亡率的最强预测因素之一。因此,开发能够评估疾病严重程度并检测 RV 功能和结构的早期适应不良变化的诊断工具非常重要。多项研究表明,诸如 N 端脑钠肽前体 (NT-proBNP)、肌钙蛋白 I、金属蛋白酶-1 和-2 的组织抑制剂以及胰岛素生长因子结合蛋白-2 等生物标志物与以下患者的预后较差有关。PH领域需要更多的研究来确定新的生物标志物,以进一步提高诊断检查的准确性。此外,目前还没有明确的病理性心肌重构和心肌纤维化的生物标志物。
众所周知,右心衰竭(RV)是肺动脉高压(PAH)死亡率的最强预测因素之一。因此,开发能够评估疾病严重程度并检测 RV 功能和结构的早期适应不良变化的诊断工具非常重要。多项研究表明,诸如 N 端脑钠肽前体 (NT-proBNP)、肌钙蛋白 I、金属蛋白酶-1 和-2 的组织抑制剂以及胰岛素生长因子结合蛋白-2 等生物标志物与以下患者的预后较差有关。PH领域需要更多的研究来确定新的生物标志物,以进一步提高诊断检查的准确性。此外,目前还没有明确的病理性心肌重构和心肌纤维化的生物标志物。
软骨中间层蛋白 (CILP)1 是转化生长因子 (TGF)-β 的拮抗剂,是一种参与心肌纤维化信号传导的细胞外基质 (ECM) 蛋白。 CILP1 RNA在左心室(LV)压力超负荷和左室心肌梗死的动物模型中表达上调,主动脉瓣狭窄或心肌梗死患者心肌组织中 CILP1 蛋白水平显着升高。有趣的是,它在小鼠模型的 RNA 水平上的表达在 RV 压力超负荷中比在 LV 压力超负荷中更明显。本研究的目的是分析 RV 压力超负荷条件下 CILP1 的表达,并确定其作为病理性心肌重构和 RV 适应不良的生物标志物的潜力。
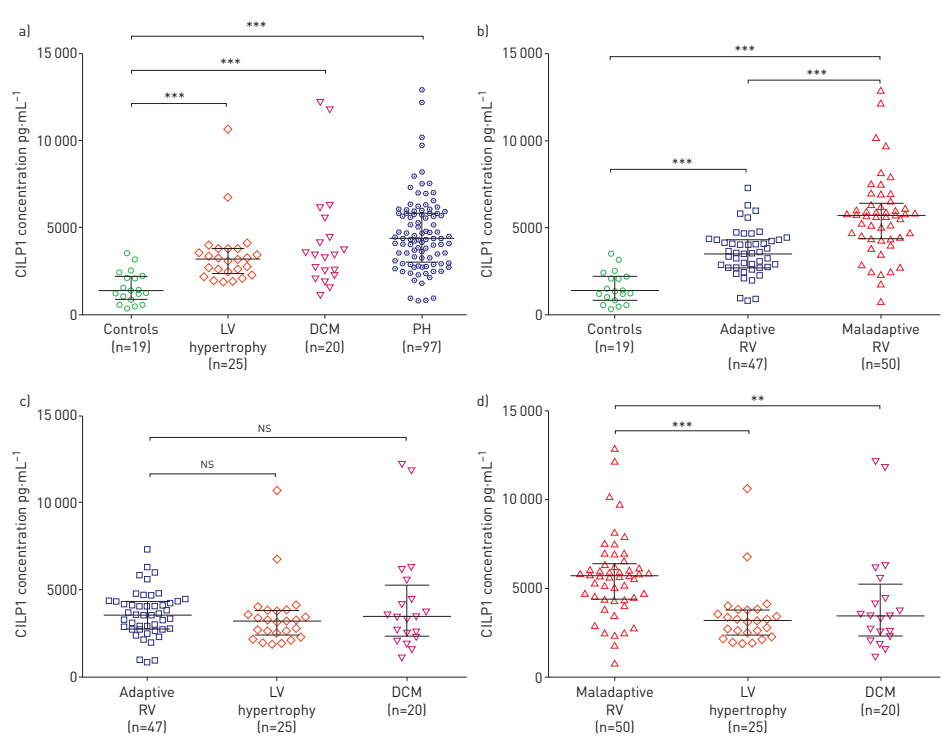
研究设计:在 14 只小鼠中进行了肺动脉结扎(PAB);另外九只老鼠接受了假手术(sham)。使用蛋白质印迹和免疫染色在所有心脏中分析 CILP1 蛋白表达。在 161 名患者中测量了 CILP1 血清浓度(97 名患有由 PH 引起的适应性和适应不良右室压力超负荷;25 名患有左心室 (LV) 肥大;20 名患有扩张性心肌病 (DCM);19 名对照者没有 LV 或 RV 异常)。
研究结果:在小鼠中,条带后 RV CILP1 的量明显高于假手术后。对照患者的 CILP1 血清水平低于所有其他组 (p<0.001)。与具有适应性 RV 功能(p<0.001)、LV 压力超负荷(p<0.001)和 DCM(p=0.003)的患者相比,右心室功能适应不良的 PH 患者的 CILP1 浓度更高。 CILP1 在接受者操作特征分析中显示出对适应不良 RV 的良好预测能力。 CILP1 和 N 端脑钠肽前体 (NT-proBNP) 的 AUC 之间没有显着差异(AUC 0.82)。高 CILP1(适应不良 RV 的临界值≥4373 pg·mL-1)与较低的三尖瓣环平面偏移/肺动脉收缩压比(p<0.001)和较高的 NT-proBNP 水平(p<0.001)相关。
研究结论:
该研究的数据表明 CILP1 作为 RV 和 LV 病理重塑的新型生物标志物的潜在作用,其与肺动脉高压环境中的 RV 适应不良和心室动脉解偶联相关。 需要进一步的研究来验证这些发现并探索导致 RV 和 LV 中 CILP1 表达潜在差异的生物分子机制。
文章出处:
Keranov S. CILP1 as a biomarker for right ventricular maladaptation in pulmonary hypertension. Eur Respir J. 2021 Apr 1;57(4):1901192. doi: 10.1183/13993003.01192-2019. PMID: 33184116.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#标志物#
92
#动脉高压#
0
#右心室#
103
#生物标志#
59
#生物标志#
83